Managing blood sugar is a grind. Honestly, if you’re living with it, you know that the "Standards of Care in Diabetes" published by the American Diabetes Association (ADA) isn’t just some dry PDF; it’s basically the rulebook for staying alive and healthy. But let’s be real. Most people don’t have time to sifting through hundreds of pages of clinical jargon. You just want to know what works. The latest ADA type 2 diabetes guidelines have shifted away from just "lowering numbers" to something much more personal. It’s about your heart, your kidneys, and frankly, your quality of life.
The old way was simple. Give everyone Metformin, tell them to walk more, and check back in three months. That’s over. Now, the ADA is pushing for "person-centered care." This means if you have a history of heart failure or chronic kidney disease (CKD), your treatment plan should look radically different from someone who doesn’t.
The Big Shift in Medication Priorities
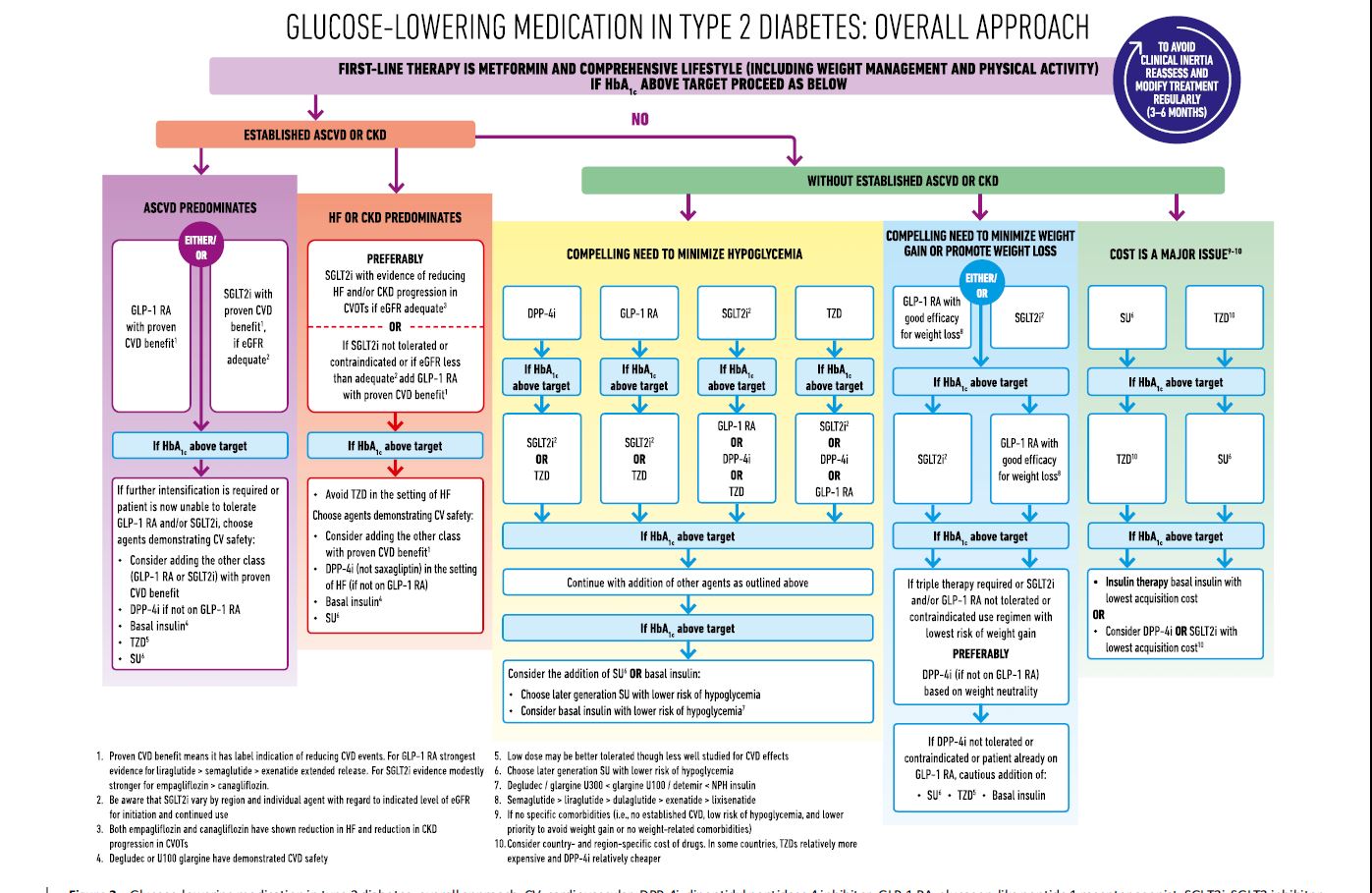
For a long time, Metformin was the undisputed king. It’s cheap, it works, and we’ve used it for decades. It’s still a heavy hitter, but the ADA type 2 diabetes guidelines now emphasize starting with SGLT2 inhibitors or GLP-1 receptor agonists if you have high-risk factors.
Why? Because these drugs do more than just drop your A1C.
📖 Related: The Most Beautiful Vagina: Why Variety is Actually the Standard
Take the SGLT2 inhibitors, like Jardiance (empagliflozin) or Farxiga (dapagliflozin). They literally make you pee out extra glucose. But the real magic discovered in trials like EMPA-REG OUTCOME is how they protect the heart. If you've got heart failure, these aren't just "diabetes drugs" anymore; they're survival tools. The ADA is very clear: if you have established cardiovascular disease, these should be on the table regardless of whether your A1C is already at target.
Then you’ve got the GLP-1s. You’ve definitely heard of Ozempic (semaglutide) or Mounjaro (tirzepatide, which is technically a dual GIP/GLP-1). These mimic hormones in your gut. They slow down stomach emptying and tell your brain you’re full. The 2024 and 2025 updates to the guidelines have leaned heavily into these for weight management. Weight loss isn't just a side effect anymore; it’s a primary goal of the treatment.
Is Metformin Dead?
Not even close.
It’s still the starting point for most. But the conversation has changed from "Metformin first, no matter what" to "What else does this patient need?" If you’re struggling with obesity, the ADA now suggests prioritizing medications that have "high to very high" weight loss efficacy. We’re talking about 15% to 20% body weight reduction, which was previously only seen with bariatric surgery.
Rethinking the A1C Goal
We’ve been told for years that 7% is the magic number. The ADA type 2 diabetes guidelines still use 7% as a general target for many non-pregnant adults, but there’s a lot of "it depends" in the fine print.
If you’re young and newly diagnosed, your doctor might push for a 6.5% goal. Why? To prevent complications decades down the line. But if you’re 85, have had diabetes for 40 years, and struggle with hypoglycemia (low blood sugar), aiming for a 7% might actually be dangerous. For older adults, an 8% or even 8.5% might be the "healthier" target because a fall caused by a dizzy spell from low blood sugar is often more dangerous than a slightly higher A1C.
It’s all about the "hypo" risk. Lows are scary. They mess with your head and your heart rhythm. The current guidelines prioritize drugs that don’t cause hypoglycemia—meaning less reliance on older sulfonylureas like glipizide if better options are available and affordable.
Technology is No Longer Optional
If you're still pricking your finger six times a day, you might be living in the past. The ADA is now much more aggressive about recommending Continuous Glucose Monitors (CGMs).
- Dexcom and Abbott’s Libre have changed the game.
- The guidelines now suggest CGMs for anyone on intensive insulin therapy.
- Even for those on basal insulin or just oral meds, a CGM can provide "Time in Range" (TIR) data.
TIR is the new A1C. Instead of a three-month average that hides the highs and lows, TIR tells you what percentage of the day you were between 70 and 180 mg/dL. The goal for most is above 70%. It’s a much more visual, immediate way to see how that sourdough toast actually affects you.
The Lifestyle Piece (It’s Not Just "Eat Less")
"Diet and exercise" is the most annoying advice ever given. It’s vague and unhelpful. The ADA type 2 diabetes guidelines try to get more specific, but they also admit there is no single "diabetes diet."
You can do Mediterranean. You can do low-carb. You can do vegetarian. The best diet is the one you actually stick to. However, the emphasis has shifted heavily toward protein quality and minimizing ultra-processed foods.
Sleep is also a huge pillar now. Did you know that poor sleep (less than 6 hours or more than 9) is directly linked to insulin resistance? The ADA now formally recognizes sleep health as part of the "whole person" approach. If you’re snoring loudly, you need a sleep apnea test. Period. Because if you have untreated apnea, your blood sugar will stay high no matter how much insulin you take.
Screening: Don’t Ignore the Organs
The ADA updated the screening intervals for a few things recently. You need your urine checked for albumin (a protein) and your blood checked for eGFR (kidney function) at least once a year. If you already have kidney issues, it might be twice or four times a year.
The eyes matter too. But here’s a kicker: if your last eye exam was normal and your blood sugar is well-controlled, you might be able to skip a year and go every two years instead of every single year. That’s a small win for your schedule.
💡 You might also like: Why You’ll Likely Fail to Match Each of the Following Arteries With Its Correct Description (And How to Fix It)
But the biggest "hidden" screening? Non-alcoholic fatty liver disease (NAFLD), now often called MASLD. The guidelines now suggest screening for liver fibrosis in people with type 2 diabetes who have elevated liver enzymes or fatty liver on ultrasound. Your liver and your pancreas are neighbors; when one is unhappy, the other usually is too.
The Cost Conversation
Let’s be honest. These new drugs like Mounjaro or Ozempic are expensive. Insurance companies love to play gatekeeper. The ADA type 2 diabetes guidelines explicitly state that clinicians must consider the "social determinants of health."
This is doctor-speak for "can you actually afford this?"
If a fancy GLP-1 costs $1,000 out of pocket, it’s not a good treatment for you. The guidelines encourage doctors to look at cost-effective alternatives, like older biosimilar insulins or even the tried-and-true Metformin/Pioglitazone combos if that’s what keeps the patient from going bankrupt.
Practical Steps for Your Next Appointment
Don't just sit there while your doctor rattles off numbers. Use the guidelines to advocate for yourself.
- Ask about your heart and kidney risk. Say: "Based on the latest ADA guidelines, am I on the best meds to protect my kidneys and heart, even if my A1C is okay?"
- Request a CGM trial. Most insurance companies are loosening up. If you're on any insulin, you have a strong case.
- Review your "Time in Range." If you have a CGM, stop obsessing over the A1C and look at your 14-day patterns.
- Discuss weight goals specifically. If you have 20 pounds to lose, ask which medications in the current guidelines provide the most "weight loss efficacy."
- Check your liver. Ask if you need a FIB-4 score calculation to check for liver scarring.
Diabetes management is a marathon. The rules change as we get better data. Ten years ago, we didn't think about "cardioprotection" nearly as much as we do today. Now, it's the center of the universe. Stay informed, stay vocal, and remember that the guidelines are a floor, not a ceiling. You and your doctor decide how high to build from there.