You’re sitting at the kitchen table. It’s quiet. There’s a stack of paper in front of you that feels heavier than it actually is. It’s the advance healthcare directive forms your doctor mentioned, or maybe your lawyer, or perhaps a pushy relative who just watched a medical drama and got spooked. You’re looking at these boxes and lines, realizing they’re asking you to predict the future. Specifically, a future where you can’t speak for yourself. It’s heavy stuff.
Most people treat these forms like a grocery list. Check a box for "no intubation," check another for "organ donor," and call it a day. That’s a mistake. A big one.
Honestly, the paperwork is just the tip of the iceberg. An advance directive isn't a "set it and forget it" document. It’s a living map for a territory you hope you never have to visit. If you fill it out wrong, or if you leave it in a desk drawer where nobody can find it, it’s basically useless. I’ve seen families tear themselves apart in hospital hallways because Mom’s directive was too vague, or because she picked the wrong person to be her "healthcare proxy." It’s messy. It’s emotional. But we need to talk about it properly.
Why Your Advance Healthcare Directive Forms Might Fail You
Legal documents are weird. They use words like "persistent vegetative state" and "terminal condition" as if those things are always clear-cut. They aren't. In the real world, medicine is gray.
A study published in the Journal of the American Geriatrics Society found that even when people have these forms, their surrogate decision-makers often struggle to predict what the patient would actually want in a specific moment. Why? Because the forms are often too clinical. They don’t capture your values. They don’t explain why you’d choose one path over another.
If you just sign a standard form without talking to your family, you’re leaving them with a riddle. They’re standing over a hospital bed, looking at a piece of paper, and trying to guess if "no heroic measures" applies to a temporary infection or just the end of the road.
The Proxy Problem
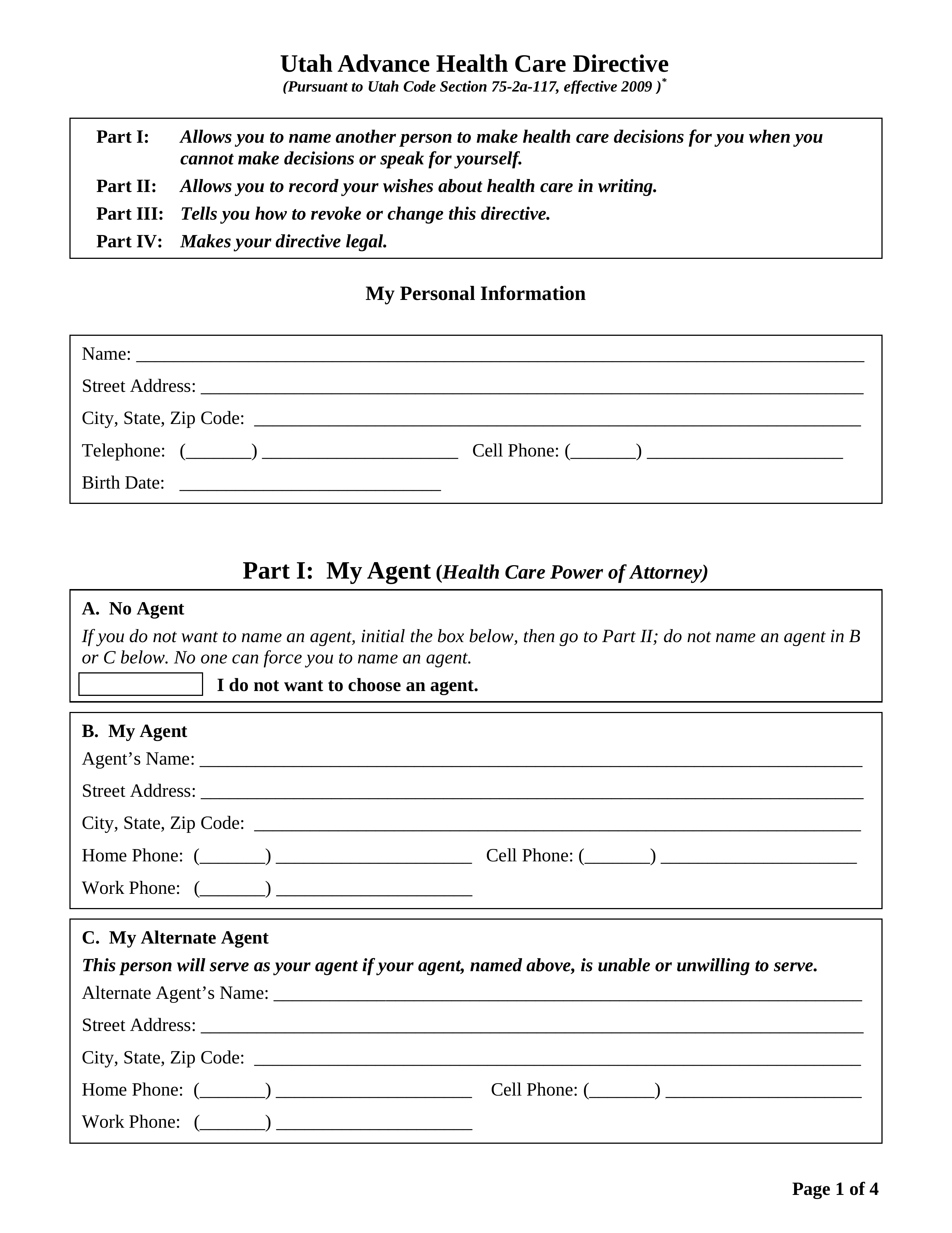
Most advance healthcare directive forms have two parts: the Living Will (what you want) and the Durable Power of Attorney for Healthcare (who speaks for you). People usually spend all their time on the first part and breeze through the second.
Bad move.
Your "proxy" or "agent" is the most important part of this whole equation. People often pick their spouse or their eldest child out of a sense of duty. But is that person actually capable of making a life-or-death decision under immense pressure? Can they stand up to a doctor who might be pushing for a procedure you don't want? Can they handle your other siblings screaming at them in the ICU?
You need a bulldog, not just a loved one. You need someone who can separate their own grief from your specific instructions.
State Variations: The Legal Maze
Here is something annoying: there is no single national form. Every state has its own rules. If you live in Florida but spend your winters in Arizona, you might need to look at both states' requirements.
Some states, like California, have very user-friendly forms. Others make you jump through hoops with multiple witnesses and notary seals. Organizations like Prepare for Your Care and the National Hospice and Palliative Care Organization (NHPCO) provide state-specific advance healthcare directive forms, but you have to make sure you’re using the most current version.
Don't just download a random PDF from 2012. Laws change. For example, some states have updated their language regarding dementia. Standard directives often kick in only when you are "terminal" or "unconscious." But what if you have advanced Alzheimer’s? You might be awake and physically healthy, but you wouldn’t want a feeding tube or aggressive antibiotics. Modern forms often include a "Dementia Provision" to cover this specific, terrifying middle ground.
The Myth of the "Do Not Resuscitate" (DNR) Order
People get this confused all the time. An advance directive is not a DNR.
A DNR is a medical order signed by a doctor. An advance directive is a legal document signed by you. If you have a heart attack at home and the paramedics arrive, they aren't going to look for your advance healthcare directive forms. They are going to start CPR. They are legally required to do so unless there is a signed, state-approved DNR or a POLST (Physician Orders for Life-Sustaining Treatment) form prominently displayed.
Realities of the Hospital Floor
Let’s get real for a second. Doctors are trained to save lives. That is their default setting. If there is any ambiguity in your paperwork, they will err on the side of "doing everything."
I remember a case—purely illustrative—where a man had checked "No" for artificial nutrition on his form. He ended up with a severe stroke. His children argued that a temporary feeding tube wasn't what he meant to refuse; they thought he just meant he didn't want to be on one forever. Because the form didn't specify "even for short-term recovery," the doctors were stuck in the middle of a family feud.
The lesson? Be specific. Instead of just checking "no," write in the margins. "I do not want a feeding tube if my cognitive function is unlikely to return to a level where I can recognize my grandchildren." That gives your proxy and your doctors a "why" to work with.
The "Five Wishes" Approach
There is a popular document called Five Wishes. It’s a type of advance directive that is legal in 46 states. What makes it different is that it uses "layman’s terms." It asks about things like:
- How comfortable you want to be.
- How you want people to treat you.
- What you want your loved ones to know.
It turns a cold legal document into something that feels human. It’s worth looking into if the standard state forms feel too robotic for you.
Digital Storage and the "Where Is It?" Crisis
You’ve filled out the forms. You’ve had them notarized. You’ve had the awkward "talk" with your kids. Now, where do the forms go?
If they stay in your safe deposit box, they are useless. If you’re in an accident on a Saturday night, nobody is getting into that bank.
- The Fridge: Paramedics are actually trained to look for medical info on the refrigerator.
- The Wallet: Carry a card that says you have a directive and lists your proxy’s phone number.
- The Portal: Upload the PDF to your hospital’s electronic medical record (EMR). This is the most effective way to ensure a doctor sees it in an emergency.
- Digital Registries: Services like MyDirectives allow you to store your advance healthcare directive forms in the cloud so they can be accessed via a QR code or a secure login by healthcare providers nationwide.
Changing Your Mind
You aren't stuck with what you decided ten years ago. Life changes. A diagnosis changes things. A divorce definitely changes things (you probably don't want your ex-spouse making your medical decisions anymore).
Review your documents every time one of the "Five Ds" happens:
- Decade: Every ten years.
- Death: Of a loved one or your named proxy.
- Divorce: Or other major family shifts.
- Diagnosis: Of a serious or chronic condition.
- Decline: Significant change in your functional health.
Just tear up the old ones and start over. Make sure everyone has the new version. It’s that simple.
Practical Next Steps
Stop thinking about this as a "death document." It’s a "quality of life" document. If you haven't started yet, here is the roadmap. No fluff, just the work.
Download the Right Version
Don't use a generic template. Go to the NHPCO website or your state’s Bar Association site to get the specific advance healthcare directive forms for your jurisdiction. If you spend significant time in two different states, get both.
Pick Your "Bulldog"
Sit down with the person you want to name as your proxy. Ask them: "If I was in a coma and the doctor said I had a 5% chance of recovery but would be severely brain-damaged, would you be able to tell them to stop life support?" If they hesitate or get too emotional, they might not be the right choice. Pick someone who can honor your wishes even when their heart is breaking.
Define Your "Red Lines"
Think about what makes life worth living for you. Is it being able to read? Recognizing your family? Not being in pain? Write these down. Use these values to guide how you fill out the sections on mechanical ventilation, dialysis, and artificial hydration.
💡 You might also like: The Best Juice for Kidney Stones: What Actually Works (and What's a Myth)
Distribute Like Crazy
Give a copy to your primary care doctor. Give one to your proxy. Give one to your alternate proxy. Keep one in your glove box or on your fridge. In the medical world, if it isn't documented and accessible, it didn't happen.
Discuss the "Gray Zones"
Talk to your doctor about what "life support" actually looks like. It’s not always a ventilator. It can be powerful antibiotics, blood transfusions, or even just high-dose pressors to keep your blood pressure up. Understanding the tools helps you decide which ones you’re okay with.
Filling out advance healthcare directive forms is an act of love for your family. It spares them the soul-crushing guilt of wondering if they made the "right" choice during a crisis. You’re giving them the gift of certainty. Do the paperwork, have the hard conversation, and then go back to living your life knowing you've handled your business.