You’re lying in bed at 2:00 AM. Your chest feels like it’s being squeezed by a hot vice, and that sour, metallic taste of stomach acid is creeping up the back of your throat. It’s terrifying. Honestly, in that moment, it feels like a heart attack. You might wonder, can acid reflux disease kill you, or is this just the price of that extra slice of pepperoni pizza? It’s a heavy question. Most people treat GERD (Gastroesophageal Reflux Disease) like a nagging annoyance—something you solve with a chalky tablet and a shrug—but the reality is more layered than a simple "yes" or "no."
The short answer is that acid reflux won't strike you down like a lightning bolt. It isn't a "drop dead" kind of disease. But if we’re being real, the long-term complications are where things get dicey. We’re talking about years of chronic inflammation that can eventually lead to life-threatening conditions. It's the slow burn that matters.
👉 See also: Curl de bicep martillo: Por qué tus brazos no crecen y cómo arreglarlo hoy mismo
The silent transformation: When cells go rogue
The biggest fear associated with chronic reflux is cancer. Specifically, esophageal adenocarcinoma. But how do we get there? It usually starts with something called Barrett’s Esophagus.
When your esophagus is constantly bathed in stomach acid, the lining gets frustrated. It isn’t built to handle the $pH$ of gastric juices. In an attempt to protect itself, the tissue actually changes. It starts looking more like the lining of your intestines. This is Barrett’s.
According to the American Society for Gastrointestinal Endoscopy, only a small percentage of people with GERD develop Barrett’s, and an even smaller percentage of those (about 0.5% per year) progress to cancer. However, here's the kicker: esophageal cancer is incredibly aggressive. By the time most people notice symptoms like trouble swallowing or unexplained weight loss, the survival rate drops significantly.
So, while the reflux itself isn't the executioner, it's the guy who opens the door for the intruder.
Aspiration pneumonia: The danger you didn't see coming
Most people think of reflux as a downward or upward flow, but they forget about the lungs. If you have severe nocturnal reflux, you might "aspirate" stomach contents. Basically, you breathe in your own reflux while you sleep.
This is incredibly dangerous.
💡 You might also like: Electric Massager for Hands: Why Most People Are Using Them All Wrong
It can cause aspiration pneumonia, a serious lung infection. For an otherwise healthy 30-year-old, it might mean a week of feeling like death and some heavy antibiotics. But for older adults or those with weakened immune systems? It can be fatal. It’s a direct, albeit less common, way that the mechanics of reflux can lead to a terminal outcome.
Can acid reflux disease kill you through "The Great Mimic"?
One of the most dangerous things about acid reflux is that it looks, smells, and feels exactly like a cardiac event. This is why ER doctors have a specific protocol for "non-cardiac chest pain."
Imagine you’re having what you think is just another bad bout of GERD. You take an antacid. You wait. But this time, it’s actually a myocardial infarction. Because you’re used to the burning sensation in your chest, you dismiss the warning signs. You stay home. You wait too long.
In this scenario, the reflux didn't kill you—the assumption that it was reflux did. This "diagnostic masking" is a very real threat for chronic sufferers.
The physical breakdown of the esophagus
Then there are esophageal strictures. Think of your esophagus as a flexible garden hose. Every time acid burns the lining, your body tries to heal it with scar tissue. Over time, that scar tissue builds up and narrows the "hose."
It sounds minor, but it's not.
Severe strictures can lead to "food bolus impaction." That’s the medical way of saying a piece of food gets stuck in your throat and won't budge. If it’s stuck long enough, or if a doctor isn't careful during an endoscopy to clear it, you risk a perforation. A hole in the esophagus is a medical emergency. It lets bacteria and acid leak into the mediastinum—the space around your heart and lungs. That leads to sepsis. Sepsis kills.
Beyond the physical: The mental toll
We don't talk enough about the psychological impact of chronic GERD. Living in constant pain, being unable to sleep, and having your diet restricted to bland mush can lead to clinical depression and anxiety. While not a direct "cause of death" in the biological sense, the degradation of quality of life is profound.
Some studies have even looked at the link between chronic sleep deprivation from nocturnal reflux and increased risks of cardiovascular disease. If you aren't sleeping because your throat is on fire, your heart never gets a break.
Why "Wait and See" is a bad strategy
Many people rely on PPIs (Proton Pump Inhibitors) like Prilosec or Nexium for decades. They’re great for symptom control. But they don't stop the reflux; they just make the fluid less acidic.
The fluid is still coming up. It’s still irritating the tissue.
Furthermore, long-term PPI use has been linked in various studies to kidney disease, bone fractures, and B12 deficiencies. It’s a trade-off. You’re trading a burning throat for potential kidney failure down the line if you don't address the root cause—usually a hiatal hernia or a weak lower esophageal sphincter (LES).
Practical steps to stop the "Slow Burn"
If you're worried about the long-term risks, stop obsessing over "can acid reflux disease kill you" and start looking at your data.
✨ Don't miss: The Couch to 5K Treadmill Strategy: Why Indoor Training Isn't Just for Rainy Days
- Get an Endoscopy: If you’ve had reflux more than twice a week for over five years, you need a baseline look at your esophageal lining. No excuses.
- The Left Side Rule: Sleep on your left side. Due to the shape of the stomach, this keeps the "puddle" of acid below the esophageal opening.
- Watch the "Vagus" triggers: Stress isn't just in your head; it affects the vagus nerve, which controls your stomach's digestion. High stress = slow digestion = more reflux.
- The 3-Hour Gap: Don't eat within three hours of lying down. Gravity is your only friend here.
- Check for a Hiatal Hernia: Sometimes, no amount of diet change will help because your stomach is literally poking through your diaphragm. That’s a mechanical issue that might need a mechanical fix (surgery).
Actionable Insights for the Long Haul
Don't panic, but don't be complacent. The danger of acid reflux isn't a heart-attack-style sudden death. It's a thirty-year game of cellular erosion.
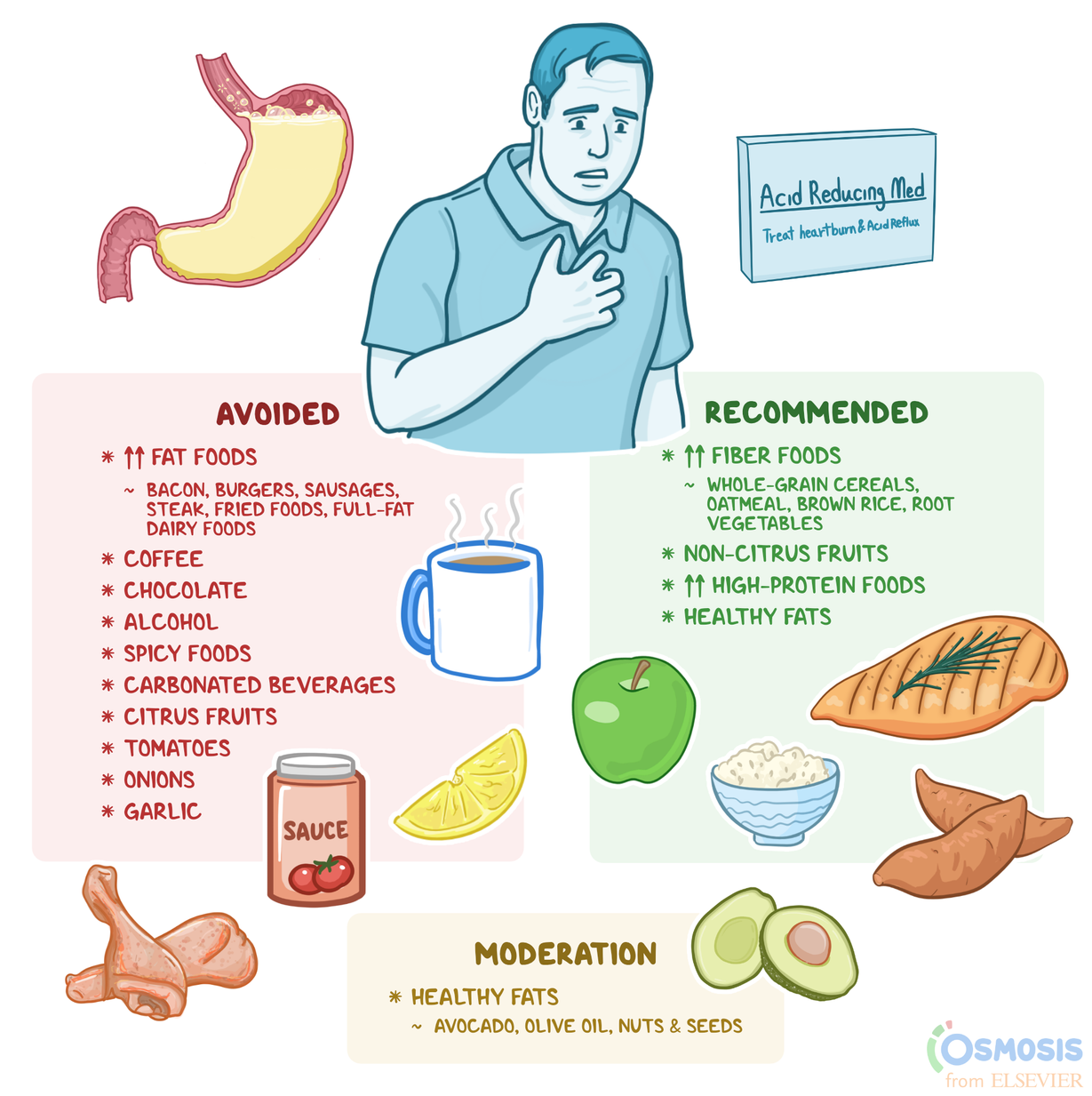
Start by tracking your triggers. It’s usually not just "acidic food." For some, it’s high-fat meals that slow down stomach emptying. For others, it’s carbonated drinks that bloat the stomach and force the LES open.
If you're over 50 and have been "living with it" for years, see a gastroenterologist. Not a general practitioner—a specialist. Ask specifically about screening for Barrett’s Esophagus. If you catch cellular changes early, they can actually "zap" them away with radiofrequency ablation before they ever turn into cancer. That is how you prevent the worst-case scenario. Be proactive, get the scope, and stop letting the "slow burn" dictate your lifespan.