Let’s be real for a second. When someone’s grandpa or grandma is rushed to the ER with a drooping face or slurred speech, "radiation" is usually the last thing on anyone's mind. You’re thinking about a stroke. You’re thinking about whether they’ll ever walk again or recognize your face. Doctors move fast. They order a CT perfusion scan because it's the gold standard for seeing which parts of the brain are dying and which can still be saved by a clot-buster or a thrombectomy. It's a lifesaver. But lately, there’s this terrifying whisper—a headline-grabbing fear—that CT perfusion radiation can kill elderly patients before the stroke even gets a chance.
Is it true? Honestly, it’s complicated.
Radiation isn't vitamins. It’s ionizing energy. When we talk about "killing" an elderly patient via radiation, we aren't usually talking about them dropping dead on the scanner table like a scene from a sci-fi horror flick. We are talking about cumulative damage, cellular stress, and the very real history of "over-beaming" accidents that have happened in major hospitals.
The GE Healthcare Legacy and the Overexposure Scandals
If you want to understand why people are scared, you have to look at what happened at Cedars-Sinai Medical Center back in 2009. This wasn't a conspiracy theory; it was a massive clinical failure. Over 200 patients were accidentally blasted with eight times the normal dose of radiation during CT perfusion scans. They started losing their hair in patches. Their skin turned red.
For an 85-year-old with thin skin and a fragile immune system, that kind of mistake is catastrophic. While the radiation itself might not cause immediate organ failure, the physiological stress of a massive radiation burn can trigger a cascade of complications in the elderly. When people search for whether CT perfusion radiation can kill elderly individuals, they are often reacting to these historical outliers where equipment was misconfigured or safety protocols were ignored.
How Much Radiation Are We Actually Talking About?
A standard CT perfusion scan delivers a dose of roughly 2 to 5 millisieverts (mSv). To put that in perspective, the average person gets about 3 mSv from the sun and the earth just by existing for a year. So, one scan is basically a year's worth of background radiation in five minutes.
That doesn't sound deadly, right?
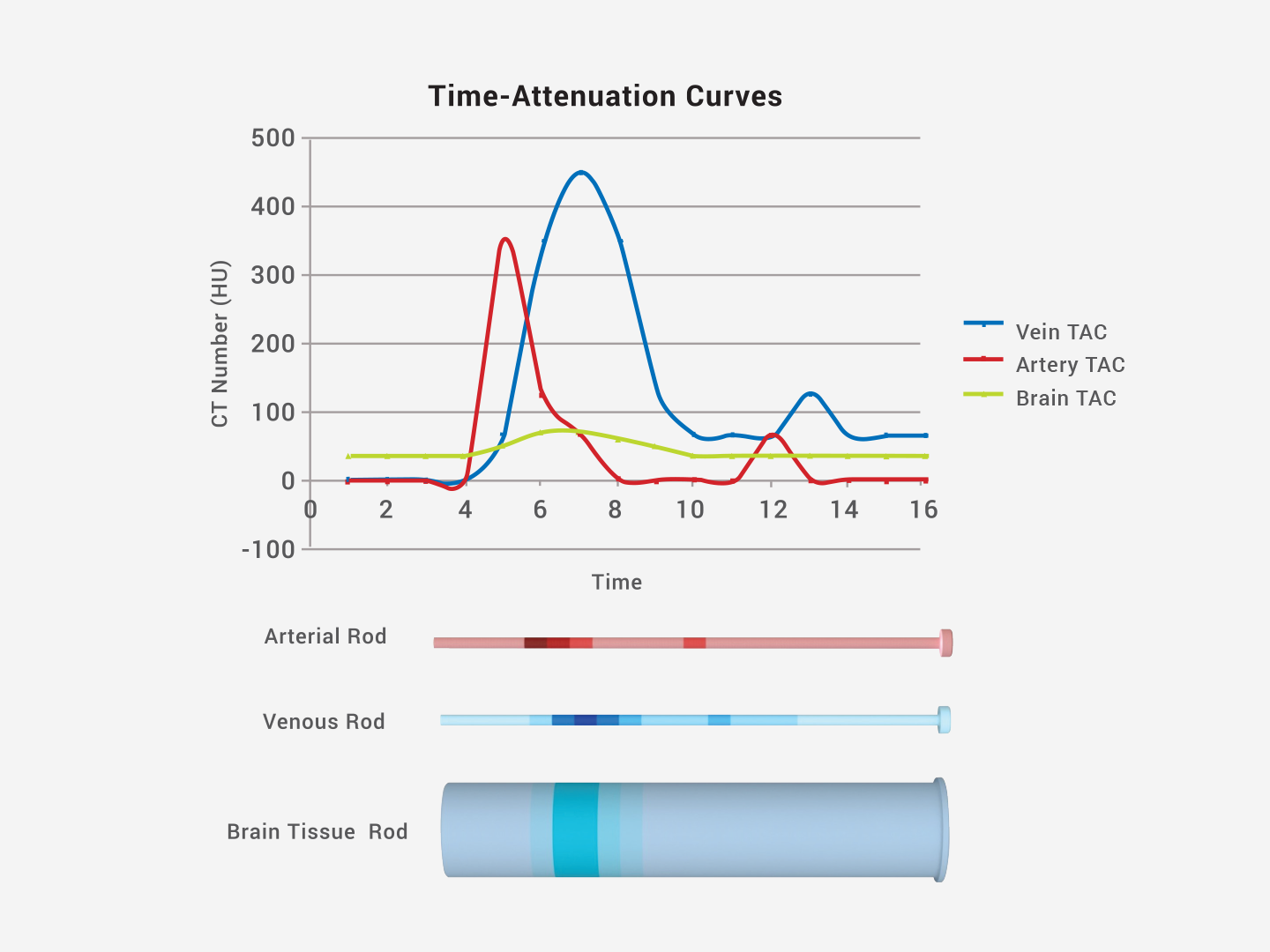
The problem is that elderly patients rarely get just one scan. They get the non-contrast CT to check for a bleed. Then they get the CT Angiogram (CTA) to look at the vessels. Then comes the CT perfusion (CTP) to check the blood flow. By the time they leave the radiology suite, they might have absorbed 15–20 mSv. In a 30-year-old, the body’s DNA repair mechanisms are robust. In an 80-year-old, those repair mechanisms are tired. They’re slow.
Why the Elderly Are at Unique Risk
Age changes the math. Biologically, older tissue is actually less sensitive to the long-term cancer-causing effects of radiation simply because cancer takes 10 to 20 years to develop, and, frankly, an 90-year-old might not have that long. But the acute effects? That's a different story.
Elderly patients often have:
- Compromised renal (kidney) function, making the contrast dye used in CTP more dangerous than the radiation itself.
- Fragile skin that can react poorly to the localized heat of high-dose imaging.
- Pre-existing neurological decline that makes "brain fog" after heavy imaging more pronounced.
There is also the "Double Jeopardy" factor. If an elderly patient is dehydrated—which is incredibly common—the combination of high-dose radiation and iodinated contrast can lead to Contrast-Induced Nephropathy (CIN). If the kidneys fail, the body can't clear toxins. That can lead to death. So, in a roundabout way, the diagnostic process, including CT perfusion radiation, can contribute to a fatal outcome in the elderly if the medical team isn't balancing the risks perfectly.
🔗 Read more: Will Probiotics Cause Bloating? What Most People Get Wrong About Gut Health
The "Stochastic" vs. "Deterministic" Problem
Medical physicists distinguish between two types of radiation damage. Stochastic effects are basically bad luck—like a stray photon hitting a DNA strand and causing a mutation that turns into cancer years later. For the elderly, doctors don't worry about this much.
Deterministic effects are the ones that happen when you hit a certain threshold. Think skin reddening (erythema) or hair loss (alopecia). These happen when the dose is too high. In the context of CT perfusion radiation, if a technician uses a "one size fits all" setting for a tiny, 90-pound grandmother, they might be delivering a deterministic dose that her body cannot handle.
Is the Risk Worth It?
Let’s be blunt: a massive stroke will kill an elderly patient much faster than a CT scan will.
Dr. Max Wintermark, a leading neuroradiologist, has spent years advocating for optimized protocols. The consensus in the medical community is that the "benefit-to-risk ratio" favors the scan. Without the CTP, doctors are flying blind. They might give a clot-buster to someone who doesn't need it, causing a fatal brain bleed. Or they might withhold a life-saving procedure because they didn't realize the brain tissue was still viable.
But "safer than a stroke" isn't the same thing as "safe."
Modern Safeguards and the "ALARA" Principle
Hospitals today are much more paranoid than they were in 2009. They use ALARA—As Low As Reasonably Achievable.
Most modern scanners have automated "dose modulation." The machine "feels" how thick the patient's head is and adjusts the X-ray beam in real-time. This is huge for the elderly. If someone has a smaller frame or thinner bone density, the machine dials back the power. This significantly reduces the chance that CT perfusion radiation can kill elderly patients or even cause minor hair loss.
📖 Related: When Dreams May Come: The Real Science of Why You Sleep-Dream at Specific Times
Real-World Precautions You Should Know About
If you are advocating for an elderly parent in the ER, you have the right to ask questions. You aren't being "difficult"; you're being informed.
- Ask if the hospital uses "dose tracking" software. Most high-level stroke centers use programs like DoseWatch or Radimetrics to ensure no patient gets an accidental overdose.
- Ensure they’ve checked the patient's creatinine levels. This is about the contrast dye, not the radiation, but they go hand-in-hand during a CTP.
- Inquire about "low-kVp" protocols. Lowering the voltage of the X-ray tube can significantly cut the radiation dose without ruining the image quality, especially in smaller elderly patients.
The Bottom Line on CT Perfusion Risks
The idea that CT perfusion radiation can kill elderly people isn't a total myth, but it’s rarely the radiation itself that does the deed. It is the context. It’s the frailty. It’s the potential for kidney failure from the dye or the rare clinical error where doses are set too high.
In a modern, accredited stroke center, the risk of dying from the radiation of a single CT perfusion scan is statistically near zero. The risk of dying from an undiagnosed or mistreated stroke is upwards of 20-30% depending on the severity.
Actionable Steps for Families and Patients
If an elderly loved one needs a CT perfusion scan, don't block it. Time is brain cells. Every minute a stroke goes untreated, two million neurons die.
Instead, follow these steps:
- Confirm the Facility: Ensure the hospital is a "Comprehensive Stroke Center" or a "Primary Stroke Center." These facilities have the most experience with CTP and the strictest radiation safety protocols.
- Mention Prior Scans: If the patient had another CT scan at a different hospital earlier that day or week, tell the doctors. Cumulative radiation is what matters.
- Hydration is Key: If they are conscious and able to swallow (and not NPO for surgery), ensure they get fluids after the scan to help the kidneys flush out the contrast.
- Monitor the Scalp: In the weeks after a stroke, check the back of the patient's head. If you see a band of hair loss, it means they received a high dose of radiation. Report this to the hospital's radiation safety officer so they can investigate their equipment settings.
Radiation is a tool. Like a scalpel, it can save a life or cause a wound. Understanding the nuance of the dose and the specific vulnerabilities of the elderly body is the only way to navigate the emergency room with confidence.