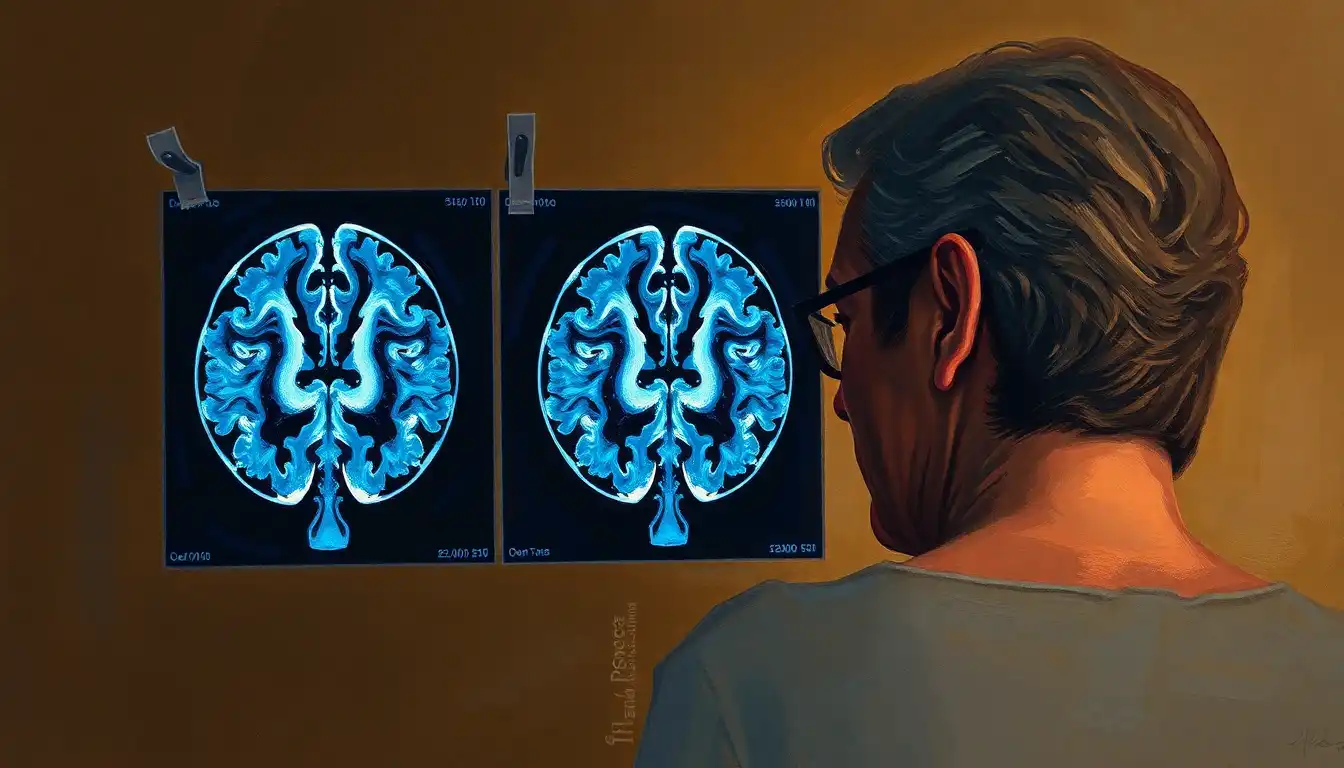
You’re sitting in a cramped consultant's office, staring at a grainy, black-and-white image of a human brain. It looks like a Rorschach test. To the untrained eye, every scan looks vaguely like a walnut. But the doctor is pointing at a dark space—a gap—and talking about "volume loss." This is the moment where the abstract fear of memory loss meets the cold reality of a dementia brain scan vs normal clinical comparison.
It’s scary. Honestly, it’s terrifying.
But here is the thing: a brain scan isn't a magic crystal ball. It’s a snapshot in time. To understand what’s happening inside someone’s head, you have to look past the pixels and understand the biology of how a healthy brain holds its shape versus how one with dementia begins to, quite literally, wither away.
The Shrinking Reality: Atrophy and the "Empty" Space
A normal brain is plump. It’s tight against the skull. Think of it like a fresh grape—firm, full, and taking up almost all the available real estate inside your head. When a radiologist looks at a healthy MRI, they see thick "gyri" (the ridges) and very narrow "sulci" (the grooves). The fluid-filled spaces in the middle, called ventricles, are small and neat.
✨ Don't miss: Why Air Quality Ventura County Residents Experience Varies So Much
Dementia changes the architecture.
In a brain affected by Alzheimer’s or frontotemporal dementia, those ridges start to thin out. The grooves get wider. It’s like the grape is turning into a raisin. This is what we call atrophy. When you compare a dementia brain scan vs normal tissue, the most striking difference is often the "black space." Because the brain tissue is shrinking, the cerebrospinal fluid moves in to fill the gaps. On a scan, that fluid looks black. So, a dementia brain often looks "holly" or "empty" in specific regions compared to the robust, light-gray mass of a healthy one.
Dr. Nick Fox, a leading researcher at University College London, has spent decades showing how these changes happen years before a person forgets where they put their keys. It’s a slow-motion collapse.
It Is Not Just About Size; It Is About Location
Where the shrinkage happens tells the story.
If you see a lot of "emptiness" in the temporal lobes—the areas right behind your ears—that’s a classic red flag for Alzheimer’s disease. Specifically, doctors look at the hippocampus. This tiny, seahorse-shaped structure is the brain’s "save button" for new memories. In a normal scan, the hippocampus is thick and sits snugly in its housing. In a dementia scan, you might see a gaping dark hole where that seahorse used to be.
But what if the shrinkage is all in the front?
That’s often Frontotemporal Dementia (FTD). These patients might have a perfectly healthy-looking hippocampus but a devastated frontal lobe. These are the people who don’t necessarily lose their memory first but might suddenly start acting rude, impulsive, or lose their ability to plan a meal. The scan reflects the behavior.
Then there’s Vascular Dementia. This one is different. It’s not necessarily about "shrinking" in a uniform way. Instead, a radiologist might see "white matter hyperintensities." On a T2-weighted MRI, these look like bright, fluffy white clouds or spots. They are essentially tiny scars from mini-strokes or "silent" plumbing issues in the brain’s blood vessels. A few spots? Normal aging. A lot of spots? That’s a sign that the brain’s wiring is being frayed by poor blood flow.
The PET Scan: Watching the Brain "Eat"
Sometimes an MRI isn't enough. An MRI shows the structure—the physical walls of the house. But a FDG-PET scan shows the activity—whether the lights are on.
Basically, the brain is a fuel hog. It runs on glucose. In a normal PET scan, the brain glows bright yellow and red because it’s hungrily devouring sugar to keep your thoughts moving. It’s vibrant. It looks alive.
When you put a dementia brain scan vs normal metabolism side-by-side, the dementia scan has "cool" spots. Blue and dark purple areas where the brain has basically stopped eating. It’s still there physically, but it’s dormant. In Alzheimer’s, this "hypometabolism" usually shows up in a very specific pattern in the posterior cingulate and parietal cortex. It’s like a map of failing power grids across a city.
Why a "Clean" Scan Does Not Always Mean You Are Fine
Here is a kicker that most people don't realize: you can have a "normal" brain scan and still have dementia.
It sounds crazy, right?
But in the very early stages—what we call Mild Cognitive Impairment (MCI)—the physical changes might be too subtle for a standard MRI to catch. The brain is incredibly resilient. It can compensate for a lot of damage before the "raisin effect" becomes obvious to a human eye. This is why clinical diagnosis depends on more than just pictures. Doctors use cognitive tests, spinal taps to look for amyloid proteins, and family interviews.
Conversely, some older people have scans that look "awful"—lots of shrinkage and white spots—yet they are sharp as a tack, running marathons and doing the Sunday crossword. This is "cognitive reserve." Their brains are built so well or have so many connections that they can handle the physical damage without losing their minds.
Scans are a tool, not a sentence.
The Future: AI and Amyloid Imaging
We’re getting better at this.
Newer scans, like Amyloid PET or Tau PET, can actually "see" the toxic proteins that cause Alzheimer’s before the brain even starts to shrink. They use a radioactive tracer that sticks to the "gunk" in the brain. If the scan glows, the gunk is there. This is a game-changer because it allows for earlier intervention, especially with the new class of drugs like lecanemab that target these specific proteins.
💡 You might also like: It Was My Birthday My Stupid Birthday: Why We Get the Birthday Blues
Also, AI is starting to beat humans at reading these things. Software can now measure the exact volume of the hippocampus down to the microliter and compare it to a database of thousands of people the same age. It’s no longer just a doctor saying, "Yeah, that looks a bit small." It’s "This brain is in the 2nd percentile for volume."
Making Sense of the Results
If you or a loved one are looking at these results, don't try to be a DIY radiologist. It’s easy to see a dark spot and panic. Most of the time, those are just "Virchow-Robin spaces," which are totally normal fluid-filled pockets around blood vessels.
The real diagnosis comes from the trend. Is the brain changing faster than it should for someone your age? That’s the question that matters.
Actionable Steps for Navigating Brain Scans
- Ask for the "Volumetric Report": If you’re getting an MRI for memory concerns, ask the doctor if they can use software like NeuroQuant or BrainCheck. These provide hard numbers on brain volume instead of just a visual "best guess."
- Check the "White Matter Burden": If the report mentions "Fazekas scale," pay attention. This measures vascular damage. Unlike Alzheimer's shrinkage, you can often slow down vascular damage by aggressively managing blood pressure and cholesterol.
- Request a 3T MRI if possible: Standard MRIs are often 1.5 Tesla (the strength of the magnet). A 3T MRI provides much higher resolution, making it easier to see tiny changes in the hippocampus.
- Contextualize with a Neuropsychological Exam: A scan is the "where," but a neuropsych test is the "how." It measures how the brain is actually performing. You need both to see the full picture.
- Look for Reversible Causes: Sometimes, what looks like dementia on a scan or in person is actually "Normal Pressure Hydrocephalus" (too much fluid) or even a severe B12 deficiency. Both can be treated.
The gap between a dementia brain scan vs normal is often a gap of years, not days. Understanding the nuances of atrophy, metabolism, and protein buildup is the first step in moving from fear to a proactive plan. A scan is just one piece of the puzzle, but it’s a powerful one for showing us exactly what we’re up against.