You’ve seen the aisles. Rows of colorful bottles promising "digestive bliss" and "immune support," some chilled in expensive refrigerators and others sitting on dusty shelves next to the multivitamins. It’s a multi-billion dollar industry built on a single, nagging question: do probiotics do anything or are we just flushing money down the toilet? Honestly, the answer is a messy "it depends." It depends on the strain, it depends on your specific biology, and it depends on whether you're trying to fix a real problem or just chasing a vague feeling of "wellness."
The logic seems sound enough. Your gut is a literal rainforest of bacteria—trillions of them. When things go sideways, you add some "good" bugs to even the score. Simple, right? Not really.
📖 Related: Pushing It Down and Praying: Why This Mental Habit is Actually Sabotaging Your Health
The Wild West of your microbiome
Most people think of their gut like a garden where you just sprinkle some probiotic seeds and wait for the flowers. It doesn't work that way. Your microbiome is more like a crowded, hyper-competitive nightclub. If you send in 10 billion Lactobacillus cells, they aren't just welcomed with open arms. They have to fight for a spot to stand. Often, they just pass through. They're tourists, not residents.
This doesn't mean they're useless. Even as tourists, these bacteria can interact with your immune system or produce metabolites that calm inflammation while they're passing through the gift shop. But the idea that a single pill will permanently rewrite your internal ecosystem is mostly a marketing fantasy.
Specificity is the only thing that matters
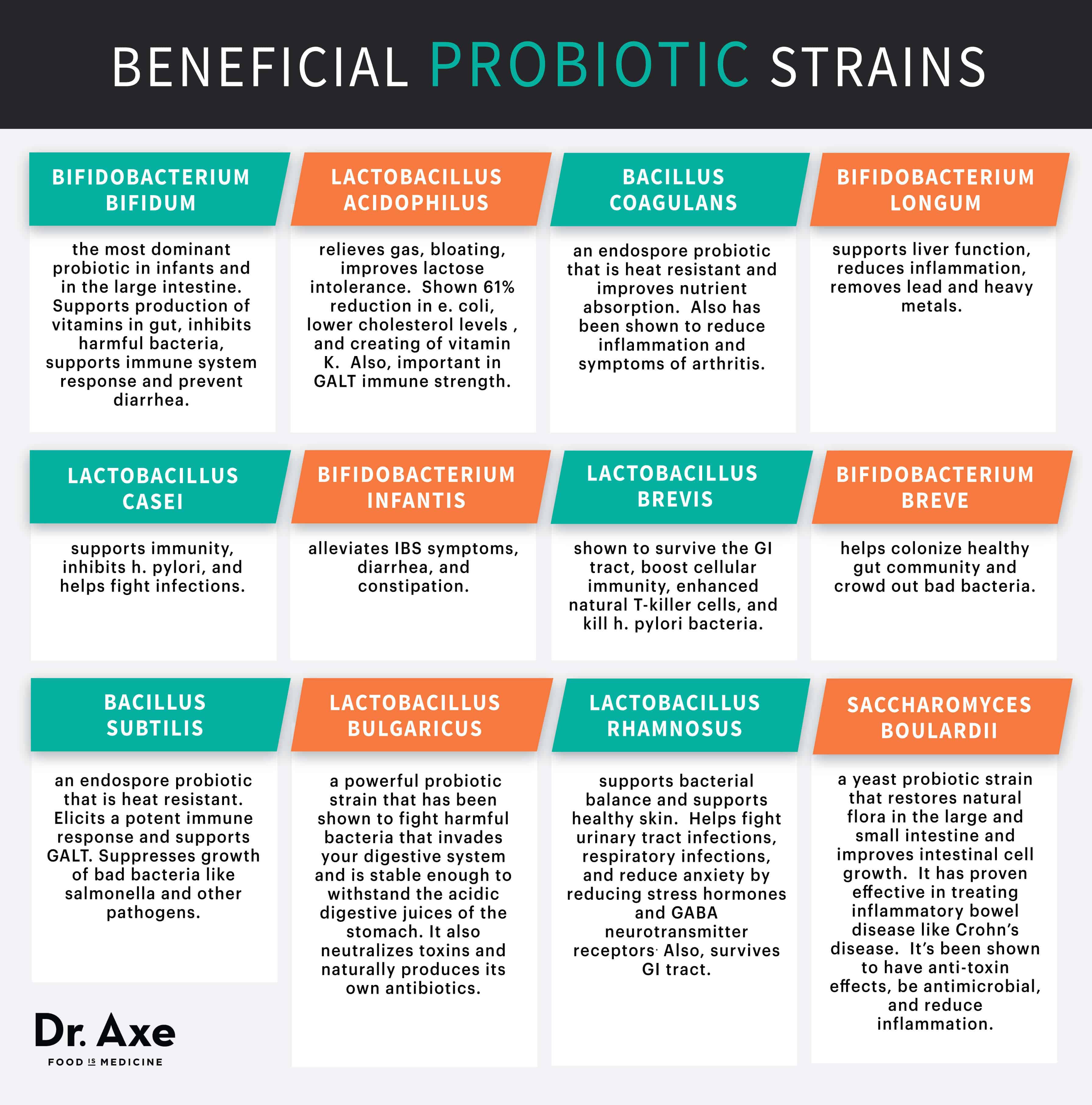
If you take a random probiotic for "bloating," you might as well be throwing darts in the dark. Science shows that benefits are incredibly strain-specific. For instance, Bifidobacterium infantis 35624 has shown real promise for Irritable Bowel Syndrome (IBS) symptoms in clinical trials. If you take a different strain, even from the same family, you might get zero results.
We have to stop talking about "probiotics" as one thing. It's like talking about "medicine." You wouldn't take a heart pill for a headache.
What the research actually confirms
Despite the hype, there are areas where the evidence is actually quite solid. We aren't just guessing anymore.
Antibiotic-Associated Diarrhea (AAD)
This is perhaps the strongest use case. When you take a scorched-earth antibiotic, it kills the bad guys but also nukes your friendly neighborhood bacteria. This vacuum often leads to diarrhea or, worse, a C. diff infection. A massive meta-analysis published in the Journal of the American Medical Association (JAMA) found that probiotics—specifically Saccharomyces boulardii (which is actually a yeast) and Lactobacillus rhamnosus GG—significantly reduce the risk of AAD. It works because you’re filling a temporary void.
Infectious Diarrhea
If you pick up a nasty bug while traveling or from a stray taco, certain probiotics can shorten the duration of the misery by about a day. It’s not a miracle cure, but when you're stuck in a bathroom, 24 hours is a lifetime.
The IBS Puzzle
IBS is where things get murky. Some patients swear by them; others feel worse. The American Gastroenterological Association (AGA) issued guidelines a few years back that were surprisingly cautious. They essentially said that for most digestive conditions, there isn't enough high-quality evidence to mandate their use, though they didn't dismiss them entirely. They’re "maybe" pills for IBS.
The dark side of the gut-brain axis
We're obsessed with "psychobiotics" now. The idea is that gut bacteria produce neurotransmitters like serotonin and GABA. It's true! Your gut produces about 90% of your serotonin. However, that serotonin doesn't necessarily cross the blood-brain barrier. So, while studies on mice show that certain bacteria make them "braver" in mazes, we are a long way from replacing antidepressants with yogurt.
Dr. Emeran Mayer, a gastroenterologist at UCLA and author of The Mind-Gut Connection, often points out that while the communication is two-way, the brain usually talks to the gut more than the gut talks to the brain. If you're stressed, your gut will hurt. Taking a pill might help the gut, but it won't necessarily fix the stressor in your life.
💡 You might also like: Does Coffee Lower Your Blood Pressure? The Surprising Truth Researchers Found
Why your expensive supplement might be failing
Most probiotics on the market are unregulated. Since they are sold as dietary supplements, companies don't have to prove they work—or even that the bacteria are alive—before putting them on the shelf.
- The CFU Trap: Companies brag about "50 Billion CFUs!" (Colony Forming Units). More isn't always better. A high dose of the wrong strain is just expensive waste.
- The Death March: Bacteria are fragile. Heat, stomach acid, and time kill them. If the bottle sat in a hot warehouse, you’re buying a bottle of dead cells.
- The Food Problem: Bacteria need to eat. If you take probiotics but eat a diet of pure processed sugar and zero fiber, those "good" bugs will starve to death before they can do anything for you.
Do probiotics do anything for the average person?
If you are generally healthy, eat a diverse diet, and don't have digestive issues, the answer is probably no. You don't need a supplement. Your body is already doing the work.
However, if you have chronic bloating, are finishing a round of penicillin, or struggle with specific GI issues, they can be a useful tool. But you have to be a detective. You have to look at the back of the bottle for the long, complicated names—not just the genus (Lactobacillus) and species (acidophilus), but the specific strain (like NCFM).
Real-world sources vs. pills
Honestly? Fermented foods are often a better bet for the average person. Kimchi, sauerkraut, kefir, and kombucha offer a "community" of bacteria rather than a monoculture. Plus, you get the nutrients from the food itself.
A study from Stanford University in 2021 found that a diet high in fermented foods increased microbiome diversity and decreased inflammatory markers more effectively than a high-fiber diet alone. That's a huge deal. It suggests that the food matrix matters. The bacteria in sauerkraut come with the fiber they need to survive. It's a packed lunch for the gut.
How to actually use this information
Stop buying whatever is on sale at the drugstore. It's a waste of money. If you want to know if probiotics do anything for your specific body, you need a protocol.
📖 Related: Mental Health Awareness Week: Why the Green Ribbon Still Matters
First, identify your goal. Are you trying to stop gas? Clear up skin? Recover from antibiotics? Once you have a goal, use a resource like the Clinical Guide to Probiotic Products (available as a website and app). It’s an independent resource that ranks brands based on actual clinical trials for specific conditions.
Second, commit to a trial period. Your gut takes time to adjust. Take the supplement for at least 4 weeks. If you don't feel a difference by then, that specific strain isn't working for you. Switch it up or stop entirely.
Third, feed the guests. You must eat "prebiotics"—things like onions, garlic, leeks, asparagus, and bananas. These are the fibers your probiotics eat. If you don't feed them, they won't stay.
Finally, keep it cold. Even if the bottle says "shelf-stable," the fridge is a safer bet for keeping those microbes alive. Heat is the enemy of life.
Actionable steps for your gut health
- Check the label for the strain: Ensure it lists three names (e.g., Bifidobacterium animalis DN-173 010), not just two.
- Time it right: Take them with a meal that contains a little bit of fat to help buffer the stomach acid, unless the instructions say otherwise.
- Diversify your ferments: Aim for three different fermented foods a week. A little bit of kimchi on your eggs, some kefir in a smoothie, or a side of real pickles.
- Track your symptoms: Use a simple note on your phone to track bloating or energy levels. If the "miracle pill" isn't doing anything after 30 days, save your $40.
- Consult a pro: If you have a compromised immune system or serious issues like Crohn’s, talk to a GI doctor before starting. In rare cases, probiotics can actually cause infections in people with weakened immunity.
The reality is that probiotics are a tool, not a cure-all. They work best when they are targeted, fresh, and supported by a diet that actually wants them there.