You've probably heard the buzz. Ketamine is the "miracle" drug for depression that works when nothing else does. But if you ask your doctor how it works, they might give you a blank stare or a very technical lecture about glutamate. Most of us grew up thinking that mental health is a simple balance of "feel-good" chemicals. We were told depression is a lack of serotonin and addiction is a surge of dopamine. Naturally, when people start talking about a dissociative anesthetic fixing treatment-resistant depression in two hours, the first question is: does ketamine affect dopamine or serotonin?
The short answer? Yes. But honestly, it’s not in the way you think. It’s way more chaotic and interesting than just "boosting" a chemical.
The Serotonin Myth and the Ketamine Reality
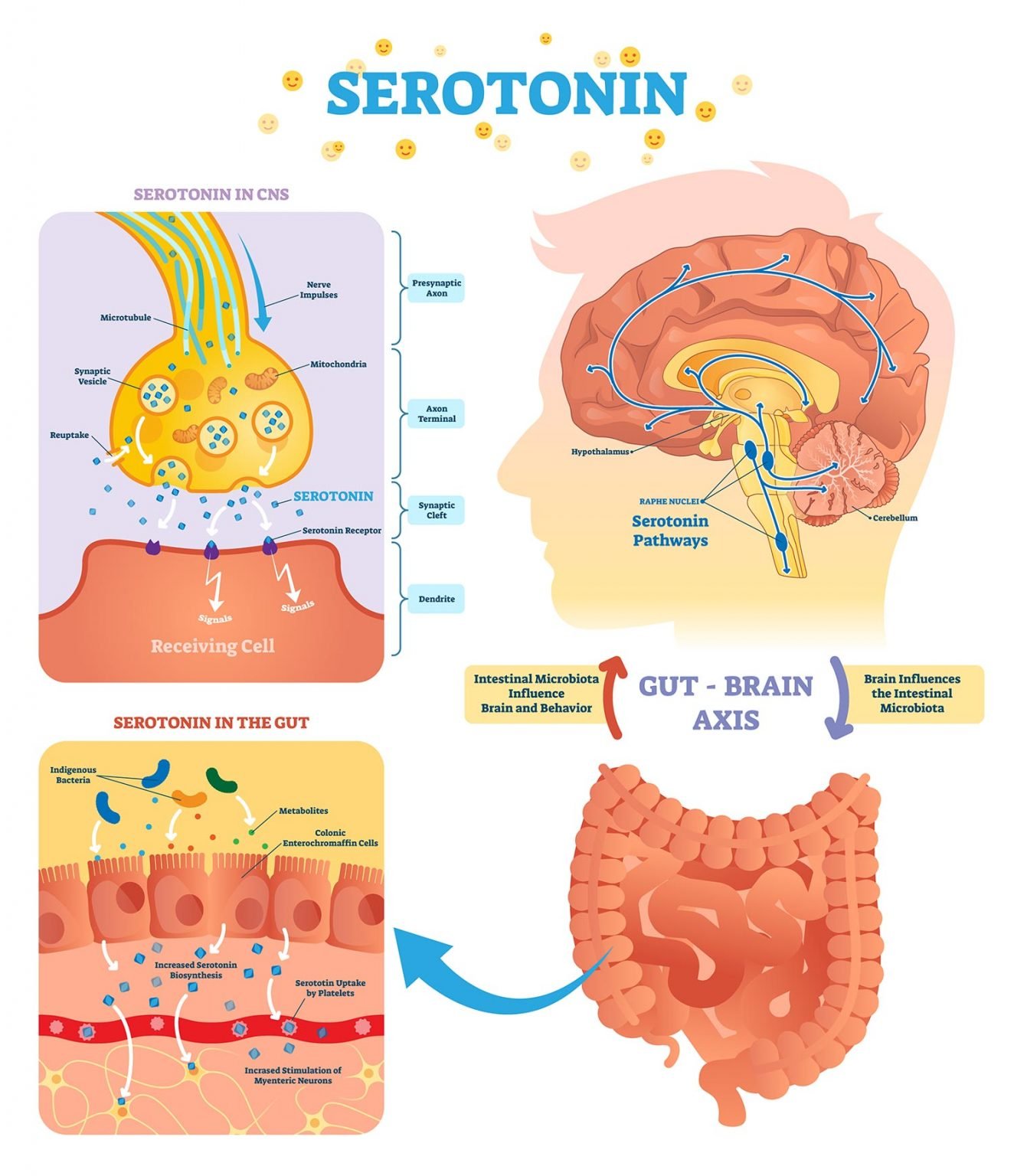
For decades, the "Chemical Imbalance" theory ruled the world. We were told that Prozac, Zoloft, and Lexapro (SSRIs) work by keeping more serotonin in the gaps between your brain cells. It sounds like a simple plumbing problem. If you’re low on the "happy chemical," just keep more of it in circulation.
Ketamine doesn't play by those rules.
While researchers like Dr. Carlos Zarate Jr. at the NIMH have spent years looking at this, they found that ketamine’s primary target isn’t serotonin at all. It’s glutamate. Glutamate is the brain’s main "on" switch. It’s everywhere.
However, recent studies from late 2024 and early 2025 have confirmed that ketamine does have a "side hustle" with serotonin. In animal models, if you chemically deplete an animal’s serotonin, ketamine’s antidepressant effects suddenly stop working. This suggests that while ketamine doesn't directly flood the brain with serotonin like an MDMA "roll," it requires a functional serotonin system to do its job.
Think of serotonin as the soil. Ketamine is the fertilizer. If the soil is completely dead, the fertilizer can’t grow anything. But ketamine itself isn't the seed; it’s the catalyst that forces the brain to start rebuilding connections—specifically by blocking NMDA receptors and triggering a "glutamate burst."
Does Ketamine Affect Dopamine? The Reward Engine
This is where things get a little spicy. If you’ve ever seen someone on a high dose of ketamine, they look like they’ve left the planet. That "k-hole" experience or the mild euphoria people feel during a clinical infusion is often blamed on dopamine.
Dopamine is the "do it again" chemical. It’s the hit of pleasure you get from a slice of pizza or a notification on your phone.
So, does ketamine affect dopamine? Absolutely.
A 2025 study using whole-brain mapping revealed that ketamine has a "divergent" effect on dopamine. Basically, it’s a bit of a weirdo. It increases dopamine release in the prefrontal cortex (the part of your brain that makes decisions and regulates mood) and the striatum (the reward center). This is likely why people feel a sudden lifting of the "gray veil" of depression. They feel motivated again. They feel... something.
But—and this is a big but—it can actually decrease dopamine activity in the limbic system, which manages fear and emotions. This weird "push-pull" might be why ketamine feels so dissociative. It’s turning up the volume on your "thinking" brain while turning down the static on your "emotional" brain.
Why This Matters for Your Brain (E-E-A-T Insights)
I've talked to researchers who are frustrated with the "serotonin vs. dopamine" debate because it ignores the actual magic of ketamine: Neuroplasticity.
When we talk about whether ketamine affects dopamine or serotonin, we’re looking at the weather. Neuroplasticity is the climate. Chronic stress and depression literally "shrivel" the synapses in your brain. It’s like a forest that’s been through a drought.
Ketamine triggers the release of something called BDNF (Brain-Derived Neurotrophic Factor). Scientists call this "Miracle-Gro for the brain." Within hours of a ketamine infusion:
- The glutamate burst happens.
- BDNF levels spike.
- Your brain starts growing new "spines" on its dendrites.
Basically, it's re-wiring the physical hardware of your brain. Traditional antidepressants are like trying to fix a computer by changing the software. Ketamine is like swapping out a fried motherboard.
👉 See also: Is There Aluminum Free Antiperspirant: What Most People Get Wrong
The Difference Between a "High" and a Treatment
One common misconception is that the "trip" is the treatment. You might think that because ketamine affects dopamine, you’re just getting high and that’s why you feel better.
Actually, the data is pretty split on this. Some studies show that people who have more intense dissociative experiences have better long-term results. Others, like a major JAMA Psychiatry trial published in late 2025, suggest that the environment and the "aftercare" (like integration therapy) matter just as much as the chemical itself.
If you’re using it recreationally, you’re hitting the dopamine system hard and fast, which can lead to addiction. If you’re doing it in a clinic, the dose is sub-anesthetic and controlled. The goal isn't the dopamine spike; it's the 48-hour window of "plasticity" that follows the infusion.
Practical Next Steps for You
If you’re looking into ketamine therapy because you’re struggling with treatment-resistant depression (TRD), don’t get too hung up on the "dopamine vs. serotonin" labels. Your brain is a symphony, not a solo.
Here is what you should actually do:
- Check your history: If you have a history of psychosis or schizophrenia, the way ketamine affects dopamine can be dangerous. Always disclose this to a provider.
- Look for "Integration": Don't just get an infusion and go home to watch Netflix. Because ketamine makes your brain "plastic," the 24 hours after a session are the best time to do therapy or start a new healthy habit.
- Ask about the "Glutamate Gap": Ask your provider how they manage the "crash" that some people feel when the initial dopamine/serotonin surge wears off.
- Monitor your bladder: Even though it helps with depression, ketamine can be hard on the urinary tract. Even at clinical doses, keep an eye on any "cystitis" symptoms.
Ketamine is a tool, not a cure-all. It uses your existing serotonin and dopamine systems to kickstart a much larger process of physical brain repair. It’s messy, it’s complicated, and it’s honestly one of the most exciting shifts in psychiatry we’ve seen in fifty years.