It starts as a tiny, annoying pinch. Maybe you're at work, or just waking up, and you realize that the bathroom trip you just took didn't feel... right. Within two hours, that pinch turns into a burning sensation that feels like passing shards of glass. If you've ever dealt with an E. coli urinary tract infection, you know exactly how fast things go south. It’s not just a "little bladder issue." It’s a full-scale invasion by a bacterium that is actually supposed to be your friend, or at least a neutral roommate in your gut.
The reality is that Escherichia coli is responsible for about 80% to 90% of all uncomplicated UTIs. That is a staggering number. While we usually associate E. coli with undercooked burgers or romaine lettuce recalls, those are specific, nasty strains. The ones causing your UTI are often your own "resident" bacteria. They just took a wrong turn at the neighborhood fork and ended up in the urethra, where they absolutely do not belong.
The Sticky Truth About Uropathogenic E. Coli
Why E. coli? Why not the thousands of other microbes floating around?
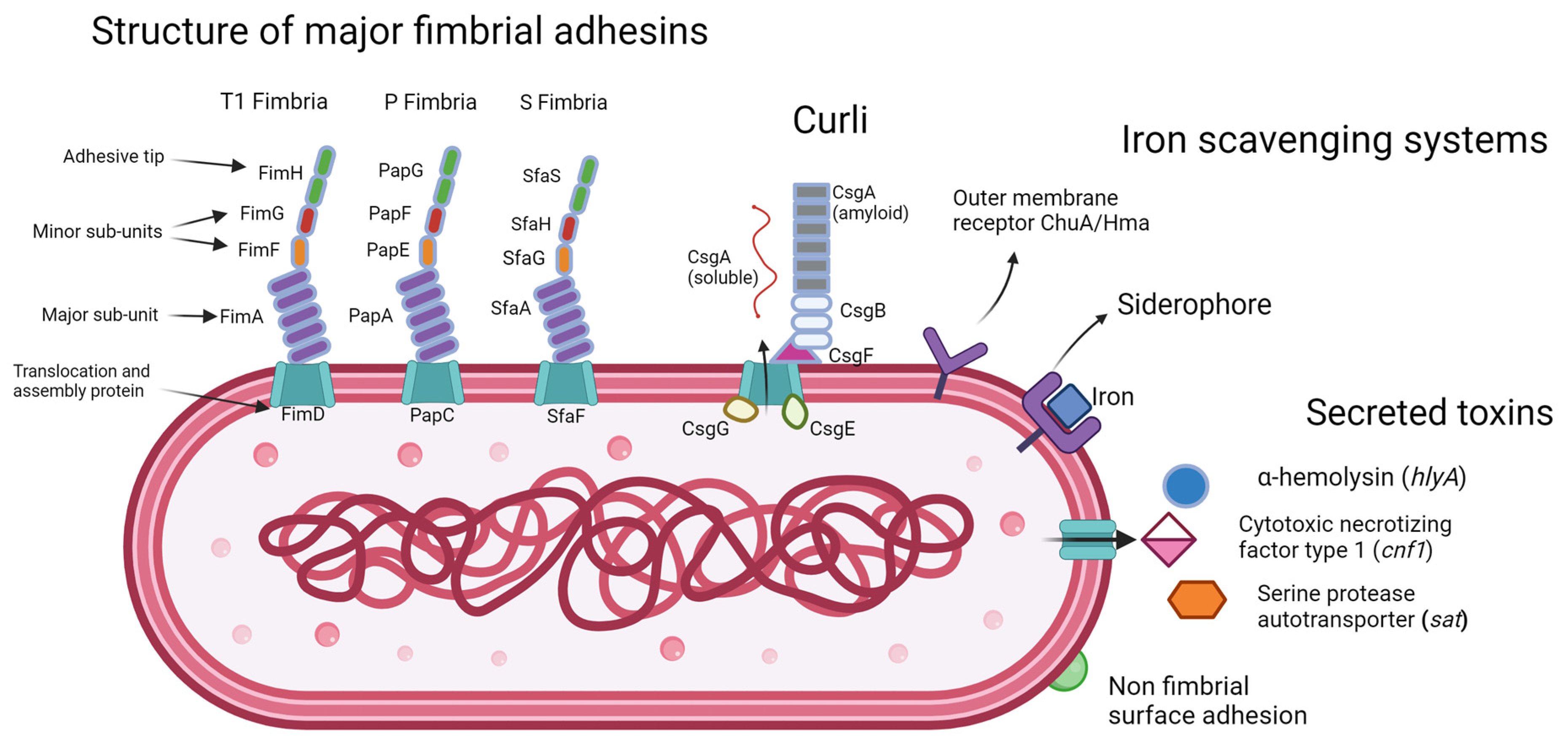
Basically, this specific type—known to scientists as Uropathogenic Escherichia coli (UPEC)—has evolved a very specific set of tools. Think of them like microscopic rock climbers. They have these hair-like appendages called fimbriae or pili. At the tips of these hairs are "adhesins" that act like superglue.
✨ Don't miss: Why is life so painful? The biology and psychology behind the hurt
When E. coli enters the urinary tract, the body tries to do the most logical thing: flush it out. You drink water, you pee, and the bacteria should go away. But UPEC doesn't play by those rules. It uses those sticky pili to grab onto the lining of the bladder (the epithelium). They latch on so tightly that the flow of urine can’t wash them away. It’s a mechanical advantage that makes them incredibly hard to evict without help.
Once they’ve anchored themselves, they don’t just sit there. They start to invade the cells of the bladder lining. They create what researchers call Intracellular Bacterial Communities (IBCs). Essentially, the bacteria hide inside your own cells. This is why some people feel like they’ve finished their antibiotics, only for the infection to roar back a week later. The medicine kills the bacteria in the urine, but the ones hiding inside the cells survive, wait for the coast to clear, and then pop back out to start the party all over again.
The Anatomy of an Invasion
It’s a short trip. For women especially, the distance from the anus (where E. coli lives happily) to the urethra is tiny. We’re talking about an inch or two of skin. That’s the "highway" for infection.
Sexual activity is a huge factor here, but it isn't the only one. Anything that moves bacteria toward the front—tight clothing, wiping the wrong way, or even just certain types of anatomy—can trigger an E. coli urinary tract infection. Men get them too, though less often. In men, a UTI is almost always considered "complicated" because the urethra is so much longer; if bacteria made it all the way up there, there might be an underlying issue like an enlarged prostate or a kidney stone acting as a breeding ground.
Symptoms That Go Beyond "Peeing a Lot"
Most people look for the classic signs: frequency, urgency, and burning. But E. coli is a bit more dramatic than that.
- Cloudy or Bloody Urine: As the bacteria damage the bladder wall, you might see "hematuria." It looks pink or even bright red. It’s terrifying to see, but it’s actually a very common symptom of a standard E. coli infection.
- The "Velcro" Pain: That heavy, dull ache in your pelvic bone (suprapubic pain) is your bladder wall being irritated and inflamed.
- The Smell: It’s hard to describe, but E. coli has a distinct, pungent, slightly "sweet but rotten" odor when it’s concentrated in urine.
If you start feeling a dull throb in your mid-back or develop a fever, the situation has changed. That’s likely the E. coli traveling up the ureters to the kidneys (pyelonephritis). This is a medical emergency. E. coli in the kidneys can enter the bloodstream, leading to sepsis. It’s not something to "wait and see" about.
📖 Related: How to Fix Stomach Pain: What Most People Get Wrong About Gut Health
Resistance is Rising
We have to talk about the elephant in the room: antibiotic resistance.
For decades, doctors just handed out Ciprofloxacin or Bactrim like candy. But E. coli is smart. It’s one of the best bacteria at sharing "resistance genes" with its neighbors. We are now seeing a massive rise in ESBL-producing E. coli (Extended-Spectrum Beta-Lactamase). This is a fancy way of saying the bacteria have learned how to create an enzyme that deactivates common antibiotics like penicillin and cephalosporins.
Honestly, it’s getting scary. In some regions, the standard "first-line" drugs only work 50% of the time. This is why your doctor might insist on a urine culture rather than just giving you a "z-pack" and sending you home. They need to know exactly which strain of E. coli you have and which drugs will actually kill it.
Cutting Through the Cranberry Myth
"Just drink cranberry juice." You’ve heard it a million times.
Does it work? Kinda. But probably not how you think.
Cranberries contain compounds called proanthocyanidins (PACs). These PACs don't actually kill E. coli. What they do is coat the bacteria so they can’t use those "sticky feet" (pili) we talked about earlier. If the bacteria can't stick, they get flushed out.
The problem? Most cranberry juice is 90% sugar and 10% juice. The sugar actually feeds the bacteria. If you’re going to use cranberry for an E. coli urinary tract infection, you need highly concentrated PAC supplements or 100% unsweetened juice that tastes like battery acid. Even then, it’s better for prevention than for curing an active infection. Once the E. coli is inside your bladder cells, all the cranberry juice in the world won’t touch it.
D-Mannose: The New Heavy Hitter
If you struggle with recurrent infections, you need to know about D-Mannose. It’s a simple sugar that occurs naturally in fruits like oranges and peaches.
Here is the cool part: E. coli loves D-Mannose. It loves it more than it loves your bladder wall. When you take a D-Mannose supplement, it passes through your kidneys and into your urine. The E. coli see the D-Mannose floating by and grab onto it, thinking it's a cell to invade. They essentially "stick" to the sugar instead of you. Then, you just pee them out.
A study published in the World Journal of Urology found that D-Mannose powder could be as effective as antibiotics for preventing recurrent UTIs, with far fewer side effects. It’s one of the few "natural" remedies that actually has solid clinical backing for E. coli specifically.
Why Some People Get Them Constantly
It feels unfair. Some people can do everything "wrong"—dehydration, wet swimsuits, lots of sex—and never get an infection. Others are hyper-vigilant and still end up at the clinic every three months.
It often comes down to genetics and the microbiome. Some people have more "receptors" on their bladder cells that E. coli can grab onto. Others have a vaginal microbiome that lacks Lactobacillus.
Lactobacillus is the "good guy" that produces lactic acid and hydrogen peroxide. This keeps the pH of the area low (acidic), which E. coli hates. If your Lactobacillus levels are low—often due to previous antibiotic use, hormonal shifts during menopause, or even certain soaps—the E. coli have an open door to migrate.
This is why "vagal seeding" with probiotics is becoming a massive area of research. We aren't just looking at killing the bad bugs anymore; we're looking at reinforcing the border wall with good ones.
Practical Steps to Stop the Cycle
If you are in the middle of a flare-up or trying to prevent the next one, stop the "slash and burn" approach of random supplements. You need a strategy.
✨ Don't miss: Finding Practice NCLEX Questions Free: What Actually Works for Passing the NGN
- Demand a Culture, Not Just a Dipstick: The little color-changing strips in the doctor's office are notoriously inaccurate. If you have recurrent E. coli urinary tract infections, you must ensure the lab grows the bacteria to see exactly what it is. This prevents "blind" antibiotic use that only breeds resistance.
- The 20-Minute Rule: If you’re sexually active, peeing within 20 minutes after sex is non-negotiable. It’s the simplest way to mechanically flush out any E. coli that got pushed toward the urethra.
- Hydration is a Math Game: You want your urine to be pale yellow. If it’s dark, the E. coli are sitting in a concentrated "soup" where they can multiply every 20 minutes. Dilute the soup.
- Check Your Biofilms: If you get infections constantly, talk to a urologist about biofilms. You might need a longer course of a specific antibiotic or a "bladder wash" to break through the protective layer the bacteria have built.
- Re-evaluate Your Birth Control: Spermicides and certain diaphragms can alter the vaginal flora and make it easier for E. coli to colonize. If you’re stuck in a loop, it might be time to switch methods.
The bottom line is that E. coli is a formidable opponent. It is literally built to survive in your urinary tract. Treating it isn't just about a 3-day course of pills; it's about understanding that your body is a complex ecosystem. You have to make that ecosystem as inhospitable to E. coli as possible while supporting the "good" bacteria that are supposed to be your first line of defense.
Don't ignore the symptoms. A "mild" bladder irritation can turn into a kidney infection or a systemic issue faster than you’d think. Listen to your body, get the right tests, and stop the invasion before it takes root.