You’re sitting in the doctor’s office. The cuff squeezes your arm tight. You see the numbers flash on the screen: 125/94. Your doctor mentions "stage two hypertension," but they focus mostly on that second digit. That 94. It’s the high bottom number blood pressure that’s causing the alarm, even though the top number looks relatively normal. Honestly? It’s a confusing spot to be in because we’ve been conditioned to worry about the big number first.
The top number is your systolic pressure. It measures the force when your heart beats. The bottom number is the diastolic pressure. It’s the pressure in your arteries when your heart is resting between beats. Think of it like a plumbing system. If the pressure stays high even when the pump isn't pushing, the pipes are under constant, relentless stress.
Isolated diastolic hypertension (IDH) is the medical term for this. It’s actually more common in younger adults—people in their 30s or 40s—than in the elderly. It’s sneaky. It doesn't usually make you feel "sick," but your blood vessels are feeling the grind every single second.
👉 See also: Creatine Explained: What the Science Actually Says About Why You Should Take It
Why the Diastolic Number Is Actually a Big Deal
Most people think of the diastolic number as the "quiet" one. It isn't. When you have high bottom number blood pressure, it often means your peripheral vascular resistance is up. Basically, your smaller blood vessels are narrowed or stiff. They aren't relaxing the way they should. This forces the heart to work harder just to move blood through the "rest" phase of the cycle.
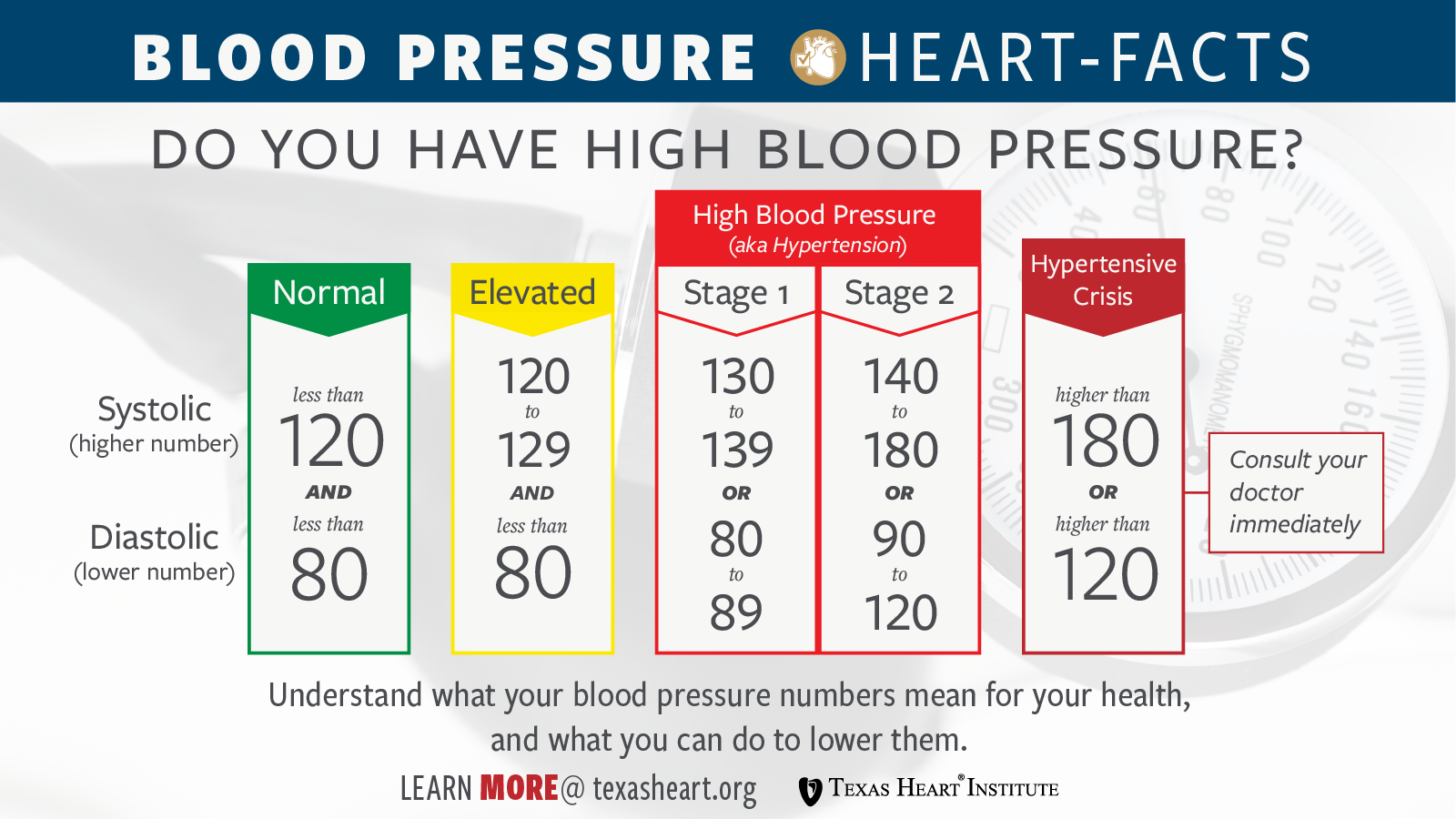
According to research published in the Journal of the American College of Cardiology, having a high diastolic reading (specifically over 80 mmHg under the newer 2017 guidelines) significantly increases the risk of cardiovascular events over time. We used to think only the systolic mattered for stroke risk. We were wrong.
While it’s true that systolic pressure tends to climb as we age and our large arteries stiffen, diastolic pressure often peaks around age 50 and then starts to drop. This is why you see "isolated systolic hypertension" in older folks. But for the younger crowd? That high bottom number is often the first red flag that the metabolic system is struggling.
The Reality of Modern Stress and Arteries
Our lives are loud. They're fast. We drink too much caffeine and don't sleep enough. This keeps our sympathetic nervous system—the "fight or flight" mode—constantly humming. When that system stays "on," your blood vessels stay constricted. That’s a direct ticket to a high diastolic reading.
I've seen patients who are fit, run marathons, and eat kale, yet their bottom number is stuck at 95. Why? Often, it’s chronic cortisol. Or maybe it's genetics. Or perhaps it's the three bags of "low-cal" popcorn they eat that are secretly loaded with sodium. Sodium is a massive driver here because it makes the body retain fluid, which increases the volume of blood the vessels have to hold during that "rest" phase.
What Causes That Bottom Number to Spike?
It’s rarely just one thing. It's a "perfect storm" of biology and lifestyle.
💡 You might also like: Watch Your Thoughts for They Become Words: Why This Old Advice Is Actually Modern Science
- Alcohol Consumption: This is a big one people ignore. Even "moderate" drinking can stiffen the arteries temporarily. If you’re drinking every night, that "temporary" becomes permanent.
- Obesity and Weight: Extra weight doesn't just sit there. It’s metabolically active. It produces inflammatory markers that tell your blood vessels to tighten up.
- Sleep Apnea: If you snore or stop breathing at night, your oxygen levels drop. Your brain panics. It sends a surge of adrenaline to wake you up. This spikes your blood pressure while you're supposed to be resting. If your diastolic is high in the morning, get a sleep study. Seriously.
- Sedentary Behavior: If you sit at a desk for 8 hours, your blood isn't circulating efficiently. Your vessels get "lazy" and lose their elasticity.
There is also a secondary cause list. Things like thyroid issues or kidney problems. If you've tried the lifestyle stuff and the number won't budge, a doctor should check your potassium and creatinine levels. It might not be "just" stress.
Dealing With High Bottom Number Blood Pressure Without Panicking
So, what do you actually do? You don't just stare at the monitor and get more stressed, which—ironically—makes the number go up. It’s called "white coat hypertension" for a reason.
The DASH Diet isn't just a buzzword. It stands for Dietary Approaches to Stop Hypertension. It emphasizes potassium, magnesium, and calcium. These minerals are like "off" switches for vessel constriction. Potassium, in particular, helps your kidneys flush out sodium. If you aren't eating bananas, spinach, or potatoes (with the skin!), you're missing out on natural blood pressure medicine.
Watch the "Hidden" Salts. It’s not the salt shaker on your table. It’s the bread. It’s the deli meat. It’s the "healthy" canned soup. Most people consume double the recommended 2,300mg of sodium daily without even trying.
👉 See also: Monte Nido Clementine Briarcliff Manor: What Really Happens Inside These Eating Disorder Programs
The Power of Zone 2 Cardio. You don't need to sprint until you puke. Brisk walking or light cycling where you can still hold a conversation—that's the sweet spot. It trains the heart to be more efficient and the vessels to dilate. Aim for 150 minutes a week. Break it up. 10 minutes here, 20 minutes there. It all counts.
Do You Need Medication?
This is the million-dollar question. If your diastolic is consistently over 90, many doctors will suggest a low-dose ACE inhibitor or a calcium channel blocker. Don't view this as a failure. Sometimes, genetics just wins. The goal of medication isn't to "fix" you forever; it's to protect your brain and kidneys while you work on the lifestyle stuff.
Some people find that losing just 5 to 10 pounds can drop that diastolic number by 5 points. That’s huge. That’s often the difference between needing a pill and staying off them.
Actionable Steps to Lower Your Diastolic Pressure Starting Today
Stop obsessing over the single "bad" reading you got at the pharmacy kiosk. Those things are notoriously uncalibrated.
- Buy a validated home monitor. Look for one that goes on the upper arm, not the wrist. Brands like Omron or Withings are usually solid.
- Take "True" Readings. Sit quietly for five minutes before you press the button. No phone. No talking. Feet flat on the floor. Take three readings, one minute apart, and average them. This is your real number.
- The 2-Gram Rule. Limit sodium to 2,000mg for two weeks. Just two weeks. See what happens to the number. Most people see a shift within days.
- Magnesium Supplementation. Talk to your doctor about Magnesium Glycinate. It’s known for helping with muscle relaxation and can sometimes take the edge off a high diastolic number caused by tension.
- Cut the Liquid Calories. Alcohol and soda are the two biggest enemies of your arteries. Try a week-long "dry" spell and watch the monitor. You might be surprised.
High bottom number blood pressure is a warning light on the dashboard. It’s not an engine failure yet. It’s your body telling you that the "rest" phase isn't restful enough. By focusing on vessel elasticity—through better minerals, less salt, and consistent movement—you can usually bring that number back into the safe zone before it causes real damage. Listen to the "quiet" number. It’s trying to tell you something important about how your body is handling the pressure of life.