The lights are too bright. Every tiny sound feels like a physical blow to your skull. If you’re asking how can i treat a migraine headache, you’re likely beyond the point of wanting a medical textbook definition; you want the pain to stop. It isn't just a "bad headache." It’s a neurological event that can derail your entire week.
Honestly, the way we talk about migraine relief is often too clinical. We focus on pills while ignoring the fact that your brain is essentially stuck in a feedback loop of hyper-excitability. Treating this isn't just about swallowing an ibuprofen and hoping for the best. It’s about a multi-pronged attack on the trigeminal nerve system.
The Immediate Response: What to Do Right Now
Stop scrolling. If the aura has started—those weird zig-zag lines or blind spots—the clock is ticking. The "golden hour" for migraine treatment is the first sixty minutes of symptom onset. This is when your brain is most receptive to abortive measures before the "central sensitization" phase kicks in, where your nerves become so sensitive that even touching your hair hurts.
Go dark. Totally dark. Research from the University of Utah Health suggests that green light is the only spectrum that doesn't significantly aggravate migraine pain, but for most people, total pitch black is the gold standard.
Temperature Therapy and Hydration
Ice vs. Heat? It’s a common debate. Most migraineurs find relief with a cold compress on the back of the neck or the forehead. This helps by constricting blood vessels and numbing the area. However, some people swear by a hot foot bath. The theory? It pulls blood flow away from the head toward the extremities.
And drink water. Not just a sip. You need electrolytes. A study published in the journal Nutrients highlighted that even mild dehydration can trigger the cortical spreading depression associated with migraines.
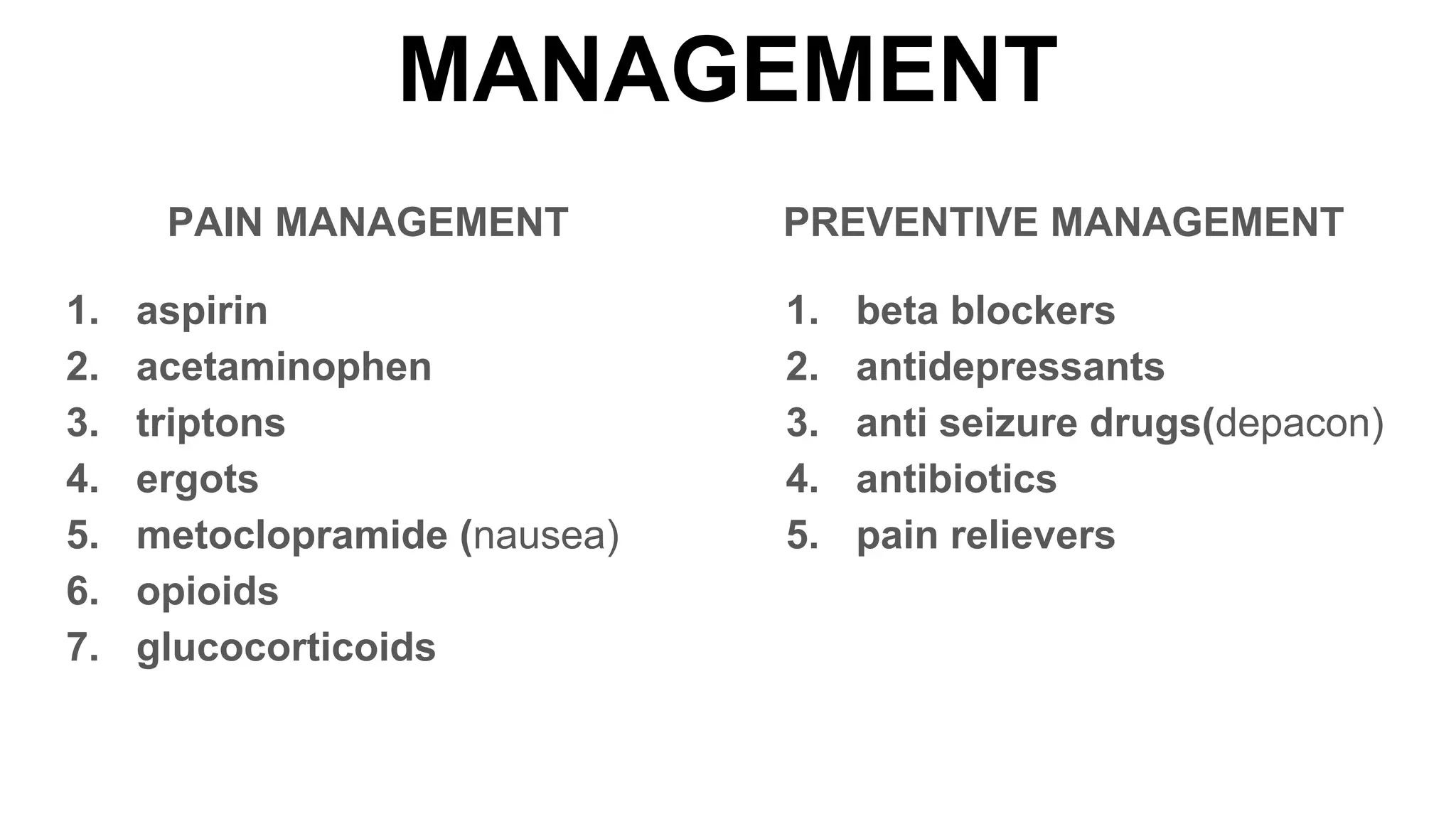
The Heavy Hitters: Pharmacological Options
You’ve probably tried over-the-counter stuff. Excedrin Migraine is basically a cocktail of aspirin, acetaminophen, and caffeine. The caffeine is the "secret sauce" here because it helps the stomach absorb the pain meds faster. But there’s a massive catch. If you use these more than two days a week, you risk "rebound headaches" or Medication Overuse Headache (MOH). It’s a vicious cycle where the medicine that fixes the pain eventually causes it.
🔗 Read more: Sleep Research News 2025 September: Why Your Brain Might Be Aging Faster Than You Think
Triptans: The Targeted Approach
When the OTC stuff fails, doctors usually move to triptans like Sumatriptan (Imitrex) or Rizatriptan (Maxalt). These aren't painkillers in the traditional sense. They work by mimicking serotonin to constrict blood vessels and block pain pathways in the brain. They are incredibly effective but can make you feel "weird"—heavy limbs, chest tightness, or a strange tingling sensation.
The New Era: Gepants and Lasmiditan
If you have heart issues or triptans don't work, there’s a newer class called Gepants (Ubrelvy, Nurtec ODT). These block a protein called CGRP (calcitonin gene-related peptide). CGRP is essentially the "messenger" that carries pain signals during an attack. By blocking the receptor, you stop the message from being delivered. Unlike triptans, these don't constrict blood vessels, making them safer for people with vascular concerns.
Natural and Neuromodulation Alternatives
Not everyone wants to live on pharmaceuticals. Some people can’t tolerate the side effects.
- Magnesium Breakthrough: There is significant evidence, supported by organizations like the American Migraine Foundation, that many migraine sufferers are deficient in magnesium. Taking 400-600mg of Magnesium Oxide or Citrate daily can reduce frequency.
- Riboflavin (B2): 400mg a day. It takes about three months to see the effect, but it helps the mitochondria in your brain cells function better.
- The Cefaly Device: This is a headband that sends tiny electrical impulses to the trigeminal nerve. It feels like a weird buzzing on your forehead. It’s FDA-cleared and can be used for both acute treatment and prevention.
Why Your Lifestyle Is the "Second Brain" of Treatment
You’ve heard it before: sleep, diet, stress. It sounds boring. It feels dismissive. But for a migraine brain, which craves homeostasis (constancy), any change is a threat.
The "Migraine Brain" is essentially a hypersensitive computer. If the "input" (flickering lights, strong smells like perfume, or a skipped lunch) is too much, the system crashes.
📖 Related: Understanding Female Anatomy: What Your Doctor Might Not Be Telling You
- The Consistent Sleep Schedule: Wake up and go to sleep at the same time every day. Yes, even on Saturdays. Sleeping in on the weekend is a classic trigger known as the "let-down headache."
- The Tyramine Factor: Aged cheeses, red wine, and cured meats contain tyramine. For some, this is a direct fuse-lighter for a migraine.
- Stress Management: It’s not the stress itself that always triggers the pain; it’s the drop in stress. Many people get migraines on the first day of vacation. This is why "winding down" slowly is actually a medical strategy.
When to Seek Emergency Help
Most migraines are benign, even if they feel like they’re killing you. But "The Worst Headache of Your Life" is a red flag. If you have a sudden "thunderclap" headache that hits peak intensity in seconds, go to the ER. If you have a fever, a stiff neck, or confusion, that’s not a migraine—that’s a medical emergency.
Actionable Steps for Long-Term Relief
If you are stuck wondering how can i treat a migraine headache every single month, you need a plan that goes beyond the current attack.
First, start a headache diary. Don't just track the pain. Track the barometric pressure, what you ate, and your sleep hours. Use an app like Migraine Buddy or just a notebook. After three months, patterns will emerge that you never noticed.
Second, schedule a "preventative" conversation with a neurologist if you have more than four "headache days" a month. You might be a candidate for Botox injections (which paralyze the nerves that signal pain) or the monthly CGRP injections like Aimovig or Emgality.
Third, check your jaw. A lot of "migraines" are actually exacerbated by TMJ (temporomandibular joint disorder). If you grind your teeth at night, your trigeminal nerve is already irritated before you even wake up. A night guard could be more effective than a bottle of pills.
Lastly, stop the "wait and see" approach. If you feel it coming on, treat it aggressively and early. The longer you wait to take your rescue medication, the less likely it is to work. Treat the brain, not just the pain.