You’re staring at the ceiling at 3:00 AM. Again. Your brain is racing through a grocery list of anxieties, your heart is thumping just a little too fast, and despite being "exhausted," you feel strangely wired. This isn't just "stress." It’s a physiological state. Most people blame their caffeine intake or a bad boss, but often, the culprit is a hormone produced by two tiny glands sitting right on top of your kidneys.
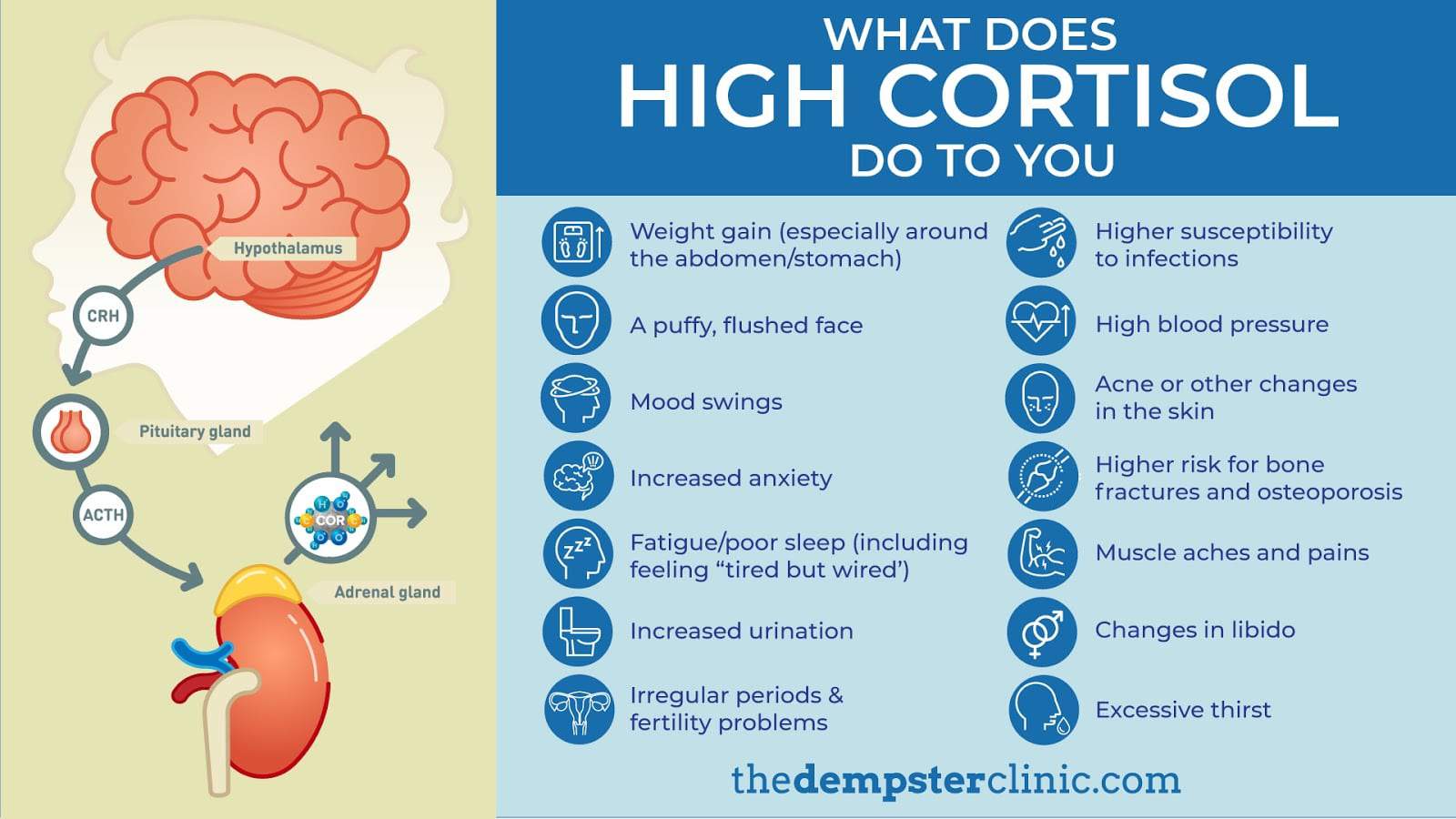
Cortisol isn't the villain it’s made out to be. We need it. Without it, you wouldn't be able to get out of bed in the morning or respond to a genuine emergency. But when the "alarm" stays on, the body starts to break down. So, how do you know you have high cortisol before it turns into a full-blown medical crisis? It’s usually not one big symptom, but a collection of subtle, annoying shifts in how your body functions.
The Midnight "Wired and Tired" Phenomenon
The most common sign is a total disruption of your circadian rhythm. Normally, cortisol should be at its peak around 8:00 AM to help you wake up and then drop to its lowest point around midnight so you can sleep. When you have chronically high levels, this curve flattens or flips. You might feel like a zombie all afternoon, reaching for a third cup of coffee, only to find that once the sun goes down, you have a second wind.
It’s frustrating.
You’re tired. You want to sleep. But your body thinks there is a predator outside the cave, so it refuses to let you drop into deep REM. Research published in The Journal of Clinical Endocrinology & Metabolism has shown that elevated evening cortisol is directly linked to fragmented sleep and insomnia. If you’re waking up between 2:00 AM and 4:00 AM with a jolt of adrenaline, that’s a massive red flag.
That Stubborn Midsection Weight
If you’ve noticed your jeans are getting tighter even though your diet hasn't changed, look at where the weight is going. High cortisol is famous for "visceral adiposity"—basically, fat stored around the organs in your abdomen.
Why? Because your abdominal fat cells have more cortisol receptors than fat cells elsewhere in the body. When cortisol stays high, it tells your body to move fat from your arms and legs and deposit it in your belly. This is a survival mechanism. It’s the body’s way of keeping energy close to the liver for quick mobilization. You might even notice your face looking rounder—a phenomenon doctors sometimes call "moon face" in extreme cases like Cushing’s Syndrome, though milder elevations cause a less dramatic puffiness.
The Weird Physical "Glubs" and Aches
- Your skin starts acting out. High cortisol inhibits collagen production. This leads to thinner skin, slower healing for small cuts, and sometimes even adult acne because cortisol triggers sebum (oil) production.
- Muscle weakness. You might feel "weak in the knees" or struggle with stairs. Cortisol is catabolic, meaning it breaks down tissues. Long-term, it can actually waste away muscle in the shoulders and thighs.
- Digestive chaos. Ever feel "butterflies" when you're stressed? That’s the gut-brain axis. High cortisol shuts down non-essential functions like digestion to prioritize "fight or flight." This can manifest as bloating, constipation, or even acid reflux.
The Brain Fog and Memory Gaps
Ever walked into a room and completely forgotten why you’re there? We all do it occasionally, but with high cortisol, it becomes a daily occurrence. The hippocampus—the part of your brain responsible for memory and learning—is incredibly sensitive to stress hormones.
According to Dr. Robert Sapolsky, a renowned neuroendocrinologist at Stanford, prolonged exposure to high cortisol can actually cause the dendrites in your brain cells to shrivel. It’s not permanent brain damage in most cases, but it makes focusing on a single task feel like trying to herd cats. You feel scattered. Irritable. Overwhelmed by things that used to be easy.
Understanding the "Stress Belly" and Blood Sugar
One of the most dangerous things about high cortisol is its relationship with insulin. Cortisol's primary job is to provide the body with glucose (sugar) to fuel a "fight." It does this by tapping into protein stores in the liver.
📖 Related: Why the Coital Alignment Technique CAT Position Is Still the Gold Standard for Intimacy
But if you aren't actually fighting a tiger—if you're just sitting at a desk stressed about an email—that extra sugar stays in your bloodstream. Your pancreas then has to pump out insulin to clear it. Over time, this leads to insulin resistance. You end up in a vicious cycle: high cortisol leads to high blood sugar, which leads to high insulin, which leads to more belly fat. This is why people with chronic stress often crave sugar and salt intensely; the body is looking for a quick energy hit to deal with the perceived threat.
Testing: Don't Just Guess
If you're wondering how do you know you have high cortisol for sure, you can’t just go by vibes. You need data. However, a single blood test at a random time of day is almost useless because cortisol fluctuates so much.
The 4-Point Saliva Test
This is often considered the gold standard for seeing the "rhythm" of your day. You spit into a tube four times: morning, noon, evening, and night. This maps your cortisol curve. If the line is flat or high at night, you have your answer.
24-Hour Urinary Cortisol
This measures the total volume of cortisol your body produces over a full day. It’s great for catching major issues like Cushing’s, but it won't show you when the spikes are happening.
Hair Cortisol Testing
This is a newer method used in research. Since hair grows about a centimeter a month, scientists can look at a strand of hair and see your stress levels from three months ago. It’s fascinating, though not yet a standard clinical tool in every doctor's office.
The Truth About "Adrenal Fatigue"
You’ve probably seen this term all over TikTok.
Honesty time: Most medical associations, including the Endocrine Society, do not recognize "adrenal fatigue" as a formal diagnosis. The idea that your adrenals just "run out" of hormones isn't supported by the data. What’s usually happening is HPA Axis Dysregulation. This is a communication breakdown between your brain (Hypothalamus and Pituitary) and your adrenal glands. Your adrenals are capable of making cortisol, but the signaling system is fried. It’s a software problem, not a hardware problem.
Actionable Steps to Bring the Numbers Down
If you suspect your levels are through the roof, don't panic. Panic just makes more cortisol. Start with these shifts:
1. Eat within an hour of waking up
Skipping breakfast or just having black coffee tells your body you're in a famine state. This spikes cortisol. Eating a meal with protein and healthy fats (like eggs and avocado) signals safety to your nervous system.
2. Stop the HIIT workouts (temporarily)
If you are already burnt out, doing an hour of high-intensity interval training is like pouring gasoline on a fire. Switch to "slow weighted workouts" or long walks. Zone 2 cardio is your friend; red-lining your heart rate isn't.
3. The "Low Information" Diet
Stop scrolling the news or social media right before bed. The combination of blue light and "outrage bait" content keeps your brain in an alert state. Try reading fiction—something that takes you out of your own reality—for 20 minutes before sleep.
4. Magnesium and Ashwagandha
Magnesium glycinate is a heavy lifter for nervous system regulation. Ashwagandha is an adaptogen that has been shown in clinical trials, like those published in the Indian Journal of Psychological Medicine, to significantly reduce serum cortisol levels in chronically stressed adults.
5. Physiological Sighs
This is a real-time tool. Inhale deeply through your nose, then take a second "sip" of air at the very top to fully expand the lungs. Exhale slowly through your mouth. Doing this three times activates the vagus nerve and can lower your heart rate and cortisol response almost instantly.
The most important thing to remember is that high cortisol is a messenger. It’s your body’s way of saying the current pace of your life is unsustainable. Listen to the small signs—the 3 AM wake-ups, the belly fat, the brain fog—before they become loud enough to ignore.
Start by tracking your sleep and energy patterns for one week. If you notice a "tired but wired" pattern, consult a functional medicine practitioner or an endocrinologist to request a saliva or urine panel rather than a standard one-time blood draw. Adjusting your light exposure by getting 10 minutes of direct sunlight in your eyes every morning can also help reset your natural cortisol rhythm without costing a dime.