You’ve probably seen the little plastic packs or heard about the "peace of mind" a tiny rod in your arm provides. But honestly, for something so common, the mechanics are kinda wild. People talk about "the pill" like it’s a magic shield. It isn’t. It’s biology. It’s chemistry. It’s basically a way of tricking your body into thinking it’s already got the situation under control so it doesn't start a new cycle.
If you’ve ever wondered how does birth control work on a cellular level, you aren't alone. It’s a mix of stopping the "go" signal, thickening the "moat," and changing the "landing pad."
The Big Three: How Your Body Gets "Tricked"
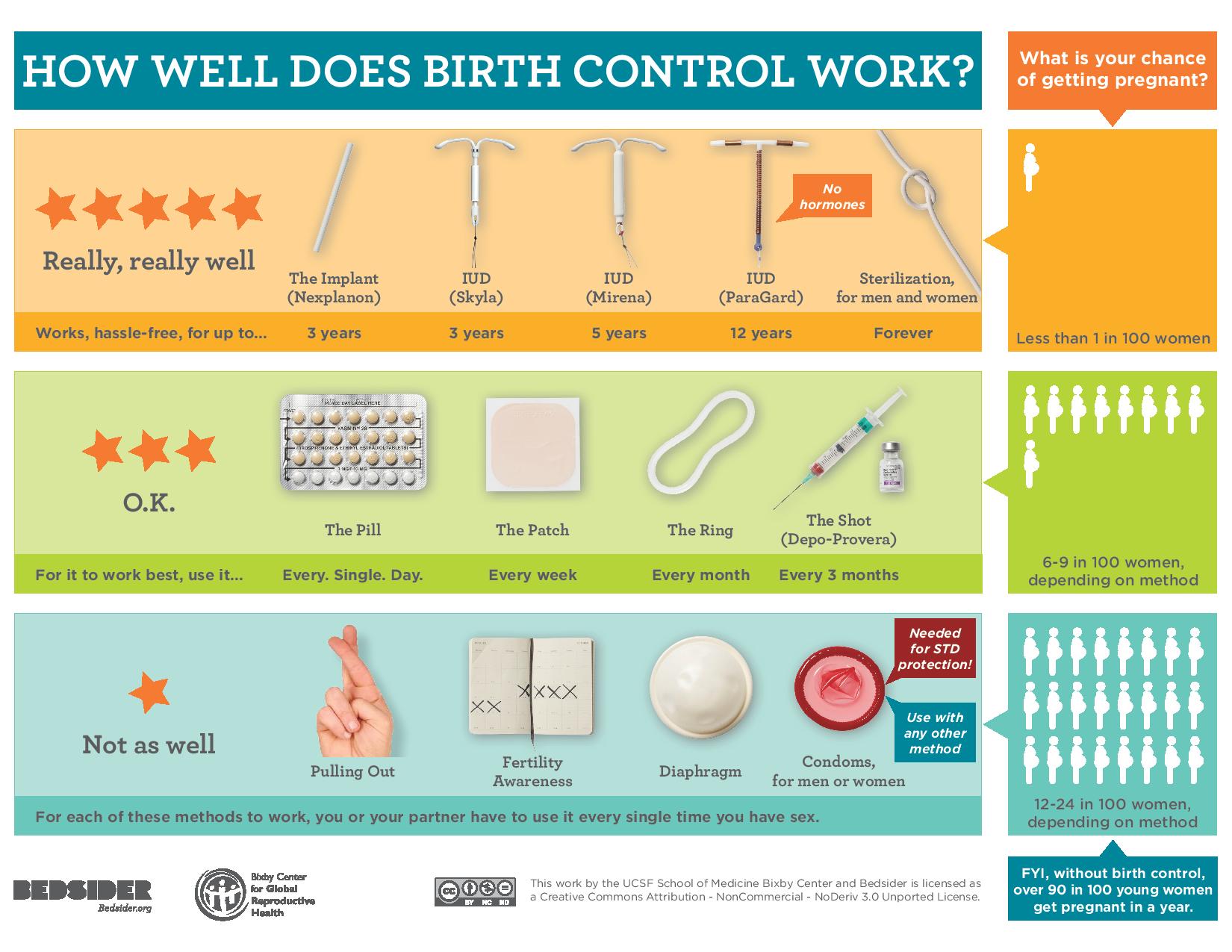
Most hormonal contraceptives—think the pill, the patch, the ring, and the shot—operate on a pretty simple premise. They use synthetic versions of hormones your body already makes: estrogen and progestin.
Here is the thing: your brain and your ovaries are in a constant, high-stakes group chat. Usually, the brain sends out Follicle-Stimulating Hormone (FSH) and Luteinizing Hormone (LH). These are the "hey, let's release an egg" signals. When you take hormonal birth control, you’re basically flooding the chat with "everything's fine, nothing to see here" messages. The brain sees the steady levels of estrogen and progestin and decides it doesn't need to send the FSH or LH signals. No signal? No egg. No egg? No pregnancy.
But that's just the first line of defense.
Nature is persistent, though. Sometimes an egg might try to sneak out. This is where the second mechanism kicks in. Progestin makes your cervical mucus thick and sticky. Think of it like turning a clear, easy-to-swim-through hallway into a room full of quicksand. Sperm can't get through that. It’s a physical-chemical barrier that most people totally forget about.
Finally, there’s the uterine lining (the endometrium). Hormones keep this lining thin. If an egg were to be released and somehow met a very determined sperm, it would need a plush, nutrient-rich environment to attach to. Birth control makes that environment more like a hardwood floor than a shag carpet. Nothing can stick.
The IUD Exception: Copper vs. Hormones
Not everyone wants hormones. Some people hate the way they feel on them, or they have medical reasons (like migraines with aura or high blood pressure) to avoid estrogen. This is where the Copper IUD (ParaGard) comes in.
It’s a tiny T-shaped piece of plastic wrapped in copper wire.
Copper is a natural spermicide. It’s not that the copper "kills" the sperm in a violent way; it just makes them dysfunctional. It causes an inflammatory response in the uterus that is toxic to sperm. They lose their ability to swim or even find the egg. It's incredibly effective, lasting up to 10 years, and it doesn't stop you from ovulating. You still have a "real" period because your cycle isn't being suppressed by hormones; the copper is just standing guard at the gate.
On the flip side, hormonal IUDs (like Mirena, Kyleena, Liletta, or Skyla) use a slow-release progestin. They mostly work by thickening that cervical mucus we talked about. For many users, they actually stop the period entirely because the lining of the uterus stays so thin there’s nothing to shed.
The "Mini-Pill" and Why Timing Actually Matters
If you’re on the combination pill (estrogen and progestin), you usually have a 12-hour "grace period" if you forget a dose. But the progestin-only pill—the mini-pill—is a different beast entirely.
You have to take it at the exact same time every day.
Why? Because the mini-pill doesn't always stop ovulation. Its primary job is thickening that mucus. That effect wears off relatively quickly. If you're three hours late, that "quicksand" starts to thin out, and the window of risk opens. It’s a high-maintenance relationship, but for breastfeeding moms or people who can't do estrogen, it’s a lifesaver.
Barrier Methods: The Low-Tech Warriors
Condoms, diaphragms, and sponges. They don’t mess with your brains or your blood. They just put a wall up.
The failure rate for these is higher, mostly because humans are... well, human. We forget. We use the wrong lubricant (oil-based lube dissolves latex, FYI). We don't leave room at the tip. According to the CDC, the "typical use" failure rate for male condoms is about 13%. Compare that to less than 1% for an IUD or the implant (Nexplanon). The implant is that tiny rod in the arm, and honestly, it’s the GOAT of effectiveness because you can't "forget" it. It just sits there, steadily releasing progestin for three years.
Emergency Contraception Isn't an Abortion Pill
There is so much misinformation here. Plan B and its generics are basically just a super-high dose of progestin.
How does birth control work when it’s "emergency" style? It delays ovulation. If the egg hasn't left the station yet, Plan B holds the train at the stop until the sperm (which can live inside you for about 5 days) die off. If you have already ovulated, Plan B likely won't work. It does not "end" a pregnancy; it prevents one from starting. This is why timing is so critical—the sooner you take it, the better the odds that the egg is still tucked away in the ovary.
The "Withdrawal" Method and "Natural" Tracking
Let's talk about the pull-out method. People laugh, but "typical use" has a failure rate of around 20-22%. In a room of five couples using only withdrawal for a year, one will likely end up pregnant. Pre-ejaculate can contain sperm, especially if a second round of sex happens shortly after the first.
Then there's Fertility Awareness-Based Methods (FABM). This isn't your grandma's rhythm method. Modern FABM involves tracking basal body temperature and cervical mucus changes. It takes a lot of discipline. You’re looking for that "egg white" consistency in mucus, which signals high fertility. It’s great for people who want to be in tune with their bodies, but it’s not exactly "set it and forget it."
💡 You might also like: Pulsera de cobre para que sirve: Lo que la ciencia y la tradición dicen realmente
Real-World Nuance: Weight, Meds, and Mistakes
Biology isn't a textbook. Sometimes things interfere.
- Antibiotics: Most don't affect birth control. The big exception is Rifampin (used for TB).
- Weight: Some studies suggest Plan B is less effective for people over 165 lbs. In those cases, the prescription pill Ella or a Copper IUD is often recommended.
- St. John’s Wort: This herbal supplement can actually make your liver process birth control hormones faster, potentially making your pill fail.
Making a Choice That Fits Your Life
Choosing a method isn't just about efficacy percentages. It's about your lifestyle. If you can't remember to take a daily vitamin, the pill is a bad idea. If you hate the idea of something being inside your uterus, an IUD is out.
If you're looking for the most "foolproof" options, LARC (Long-Acting Reversible Contraception) is the gold standard. The Nexplanon implant and IUDs remove the "human error" variable. You get it done, and you're good for years.
Actionable Next Steps:
- Check your meds: If you’re starting a new prescription, specifically ask your pharmacist if it interacts with hormonal contraceptives.
- Audit your memory: If you’ve missed more than two pills in the last three months, consider switching to the ring (once a month) or the patch (once a week) to lower the mental load.
- Get a backup: Keep a box of emergency contraception in your medicine cabinet. It’s cheaper to buy on Amazon or at a pharmacy ahead of time than to panic-buy it at 2:00 AM on a Sunday.
- Talk to a pro: Use resources like Bedsider.org or Planned Parenthood to compare methods side-by-side based on side effects like acne, weight changes, or period heaviness.
Birth control is a tool. Like any tool, it works best when you know exactly how it operates and you use the right one for the job at hand.