You feel that scratch in your throat or the heat of a skin infection and your brain immediately jumps to one thing: I need a Z-Pak. Or maybe some Amoxicillin. Honestly, we've lived in the antibiotic era for so long that we treat these pills like magic beans. But here is the reality. Treating bacterial diseases isn't just about carpet-bombing your system with meds. It's a delicate dance between killing the invader and keeping your own body from becoming collateral damage.
Bacteria are everywhere. Most are your friends. Some, like Staphylococcus aureus or Streptococcus pneumoniae, are definitely not. When they start multiplying where they shouldn't, your immune system sounds the alarm. You get the fever, the swelling, and the fatigue. That’s your body fighting. Sometimes it wins alone. Sometimes it needs help.
The first rule of how to treat bacterial diseases
Don't guess. Seriously.
The biggest mistake people make is assuming every "sick" feeling is bacterial. It's usually not. Most respiratory gunk is viral. If you take an antibiotic for a virus, you’re doing zero damage to the illness while simultaneously nuking your gut microbiome. This is how we get antibiotic resistance.
Doctors use a "culture and sensitivity" test for a reason. They take a swab, grow the bug in a lab, and then literally drop different antibiotics on it to see which one kills it. If you have a UTI, for example, a doctor might find E. coli. They then check if that specific strain is resistant to Ciprofloxacin. If it is, and they gave you "Cipro" anyway, you’d be suffering for nothing.
Why the "Full Course" actually matters
We’ve all done it. You feel better on day three, so you stop taking the pills. The bottle is half-full in your cabinet. Stop doing that. When you start an antibiotic, the "weak" bacteria die first. You feel great. But the "strong" ones—the ones with slight mutations that make them tougher—are still hanging on. If you stop the treatment early, those survivors multiply. Now you have a secondary infection that is much harder to kill.
Narrow-spectrum vs. Broad-spectrum
Think of a broad-spectrum antibiotic like a grenade. It kills everything. Doctors use these when they aren't sure what's making you sick but you're in bad shape. Drugs like Tetracycline or Amoxicillin-clavulanate (Augmentin) fall into this bucket. They are effective, but they are rough on your digestion because they kill the "good" bacteria in your intestines too.
Narrow-spectrum drugs are like snipers. Penicillin G is a classic example. It’s great for specific Gram-positive bacteria but won't touch others. Whenever possible, you want the sniper. It leaves your natural defenses intact while taking out the specific threat.
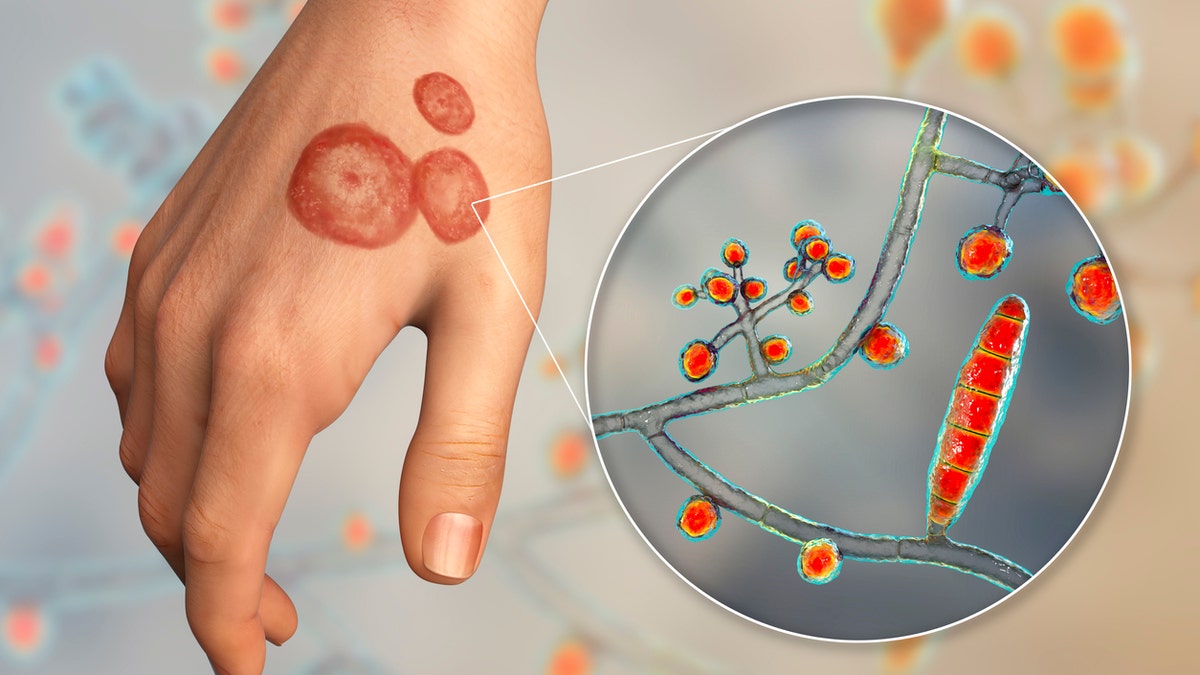
The rise of the "Superbugs"
We have to talk about MRSA (Methicillin-resistant Staphylococcus aureus). It sounds scary because it is. Decades of overprescribing antibiotics have taught bacteria how to survive our best weapons. According to the CDC, more than 2.8 million antibiotic-resistant infections occur in the U.S. each year.
Treatment for these requires "drugs of last resort" like Vancomycin. These are often administered via IV in a hospital setting. It’s a stark reminder that our arsenal isn't infinite. If we keep using heavy-duty meds for minor sinus infections, we’re going to run out of options when things get truly life-threatening.
Biofilms: The invisible shield
Some bacteria are sneaky. They create a "biofilm," which is basically a slimy protective layer that sticks to surfaces like heart valves, catheters, or even your teeth. Antibiotics often struggle to penetrate this goo. This is why chronic bacterial diseases, like certain types of Lyme disease or persistent ear infections, are so hard to kick. Treatment often involves a combination of high-dose antibiotics and sometimes physical disruption—like surgery or specialized cleaning—to break that film apart.
Supporting your body during treatment
You shouldn't just sit back and let the pills do the work. Your immune system is still the lead actor here.
- Hydration is non-negotiable. Bacteria produce toxins as they die (ever heard of a Herxheimer reaction?). You need water to flush those metabolites out through your kidneys.
- Probiotics are your best friend. Since antibiotics are a "scorched earth" policy for your gut, you need to replant the forest. Studies published in JAMA suggest that taking probiotics (specifically Lactobacillus rhamnosus GG) during and after antibiotic treatment can significantly reduce the risk of antibiotic-associated diarrhea.
- Rest. Your body diverts a massive amount of energy to the immune response. If you're hitting the gym while fighting off strep, you're stealing resources from your own defense team.
Natural adjuncts and myths
There’s a lot of "natural antibiotic" talk online. Oregano oil, garlic, manuka honey. Do they work?
Sorta.
Manuka honey has proven antibacterial properties when applied topically to wounds. It creates a barrier and has a low pH that bacteria hate. Garlic contains allicin, which shows antibacterial activity in a petri dish. But—and this is a huge "but"—eating a clove of garlic is not going to cure a kidney infection. Use these things as support, not as a replacement for medical intervention when a systemic infection is present.
Non-antibiotic treatments on the horizon
Science is getting weird (in a good way). Because of resistance, researchers are looking at Bacteriophages. These are viruses that only eat bacteria. They are incredibly specific. If you have a specific strain of Pseudomonas, doctors can potentially deploy a phage that hunts only that strain, leaving everything else alone. It’s currently used mostly in compassionate care cases, but it’s the future of how to treat bacterial diseases.
There’s also work being done on "anti-virulence" drugs. Instead of killing the bacteria, these drugs just "disarm" them. They stop the bacteria from producing toxins or building those protective biofilms. If the bacteria can't hurt you, your immune system can clean them up at its own pace without the pressure of an escalating "arms race."
💡 You might also like: Qué es glicerina y para qué sirve: Todo lo que nadie te explica sobre este líquido transparente
Actionable steps for your next infection
If you suspect you're dealing with a bacterial issue, here is the protocol that actually works and keeps you safe.
- Get a definitive diagnosis. Ask your doctor, "Are we sure this isn't viral?" Ask for a culture if the infection is persistent.
- Verify the dosage. Ensure you understand exactly when to take the medication. Some work better on an empty stomach; others need fat to be absorbed.
- Timing is everything. If the label says "every 8 hours," try to actually do it every 8 hours. You want a steady concentration of the drug in your bloodstream. Letting the levels dip gives the bacteria a chance to recover.
- Manage the gut. Start a high-quality probiotic two hours after your antibiotic dose. Continue this for at least two weeks after the prescription ends.
- Watch for "C. diff." If you develop severe, watery diarrhea or intense cramping after taking antibiotics, call your doctor immediately. Clostridioides difficile is a nasty bacterium that can take over when your good gut flora is wiped out.
- Dispose of leftovers. If you have pills left over, don't save them for a rainy day. Take them to a pharmacy "take-back" bin. Using old, expired, or partial doses later is a recipe for creating a resistant infection in your own home.
Treating a bacterial disease is a partnership between you, your doctor, and the medication. Respect the medicine, protect your gut, and never underestimate the power of a bacterium that’s fighting for its life.