Living with Crohn’s or Ulcerative Colitis is a nightmare. Honestly, there is no other way to put it. You’re constantly scanning the room for the nearest exit, wondering if that last bite of lunch is going to trigger a "flare-up from hell" that lands you in the hospital. When people start searching for an inflammatory bowel disease cure naturally, they’re usually at the end of their rope. Maybe the biologics stopped working. Maybe the side effects of prednisone—the "moon face," the insomnia, the rage—became too much to handle.
But we need to have a very real, very blunt conversation about the word "cure."
💡 You might also like: Lion’s Mane Mushroom Supplement: What People Honestly Get Wrong
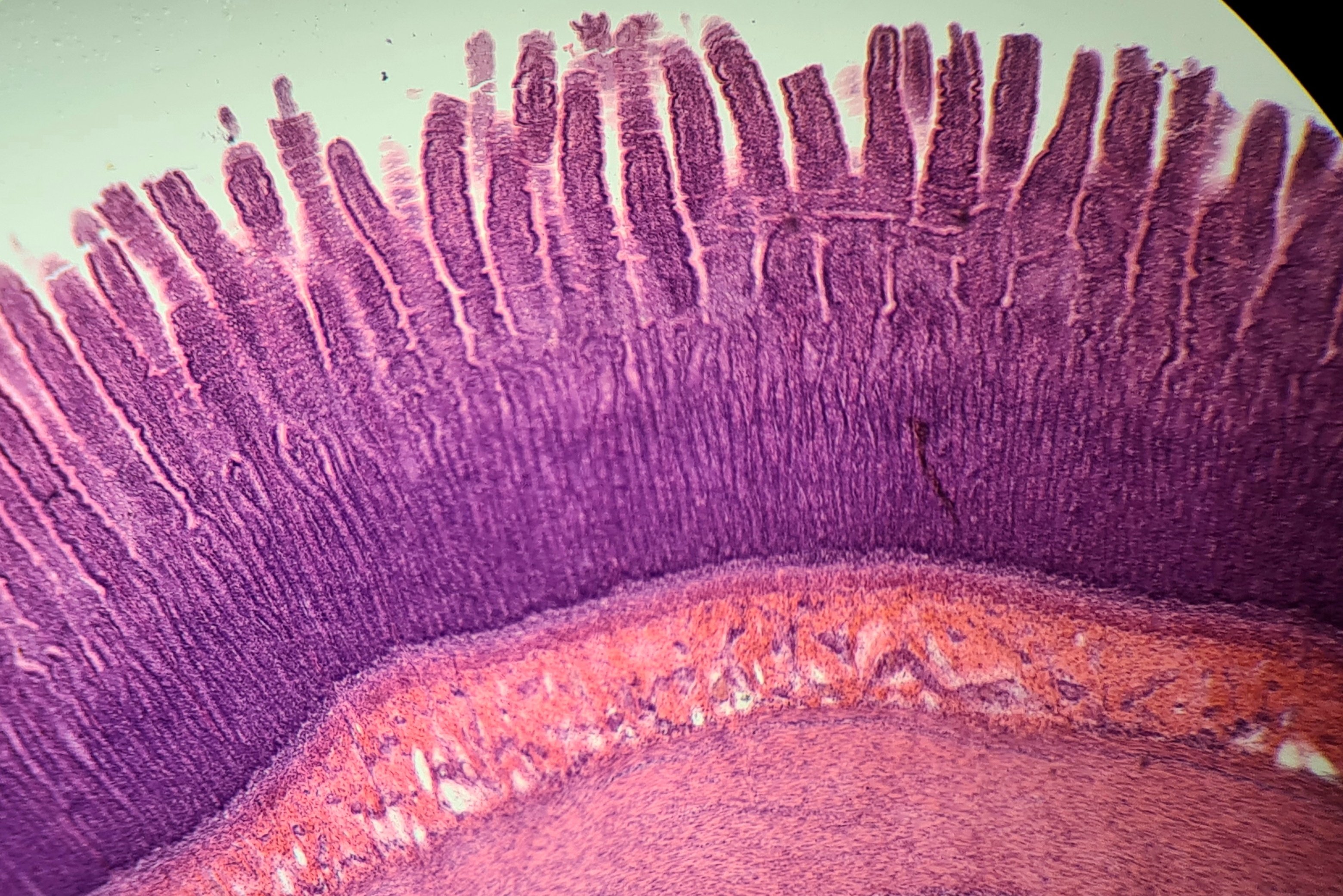
In the medical community, especially when talking to experts like Dr. Balfour Sartor at the UNC Center for GI Biology and Disease, the "C-word" is rarely used. Instead, we talk about deep mucosal healing. We talk about clinical remission. If you are looking to "cure" IBD naturally, you are looking for a way to shut down the immune system's mistaken attack on your own gut lining without relying solely on a pill or an infusion. It is possible to live a symptom-free life. It happens. But it isn't a "one-and-done" fix like healing a broken arm. It's a fundamental shift in how your body interacts with the world.
The Microbiome: Not Just a Buzzword
Your gut is an ecosystem. Think of it like a forest. In IBD, that forest is on fire. Most people think they can just take a probiotic and the fire will go out. It doesn't work that way. Research from the Human Microbiome Project has shown that people with IBD have significantly less microbial diversity than healthy people. You’re missing the "good guys" like Faecalibacterium prausnitzii, which produces butyrate—a short-chain fatty acid that basically acts as fuel for your colon cells and keeps inflammation down.
You can't just supplement your way out of a bad ecosystem.
Natural management starts with changing the soil. That means looking at the Specific Carbohydrate Diet (SCD) or the IBD-AID (IBD Anti-Inflammatory Diet). These aren't just "healthy eating." They are biological interventions. The SCD, popularized by Elaine Gottschall, focuses on removing complex carbs that the damaged gut can't break down. When undigested carbs sit in your gut, they feed the bad bacteria. Those bacteria produce toxins. Those toxins trigger your immune system. By cutting the fuel source for the "bad guys," you give your gut lining a chance to knit back together.
Why Your Doctor Might Be Skeptical (And Why That’s Okay)
Gastroenterologists are trained to follow the "Step-Up" or "Top-Down" therapy models using pharmaceuticals like Remicade or Stelara. They look at the data. And the data for "natural cures" is often messy because everyone's gut is different. What works for a guy with Crohn’s in his terminal ileum might be a disaster for a woman with Ulcerative Proctitis.
However, the tide is shifting.
Dr. James Lewis at the University of Pennsylvania led the DINE-CD study, which compared the Mediterranean diet to the SCD. Surprisingly, both diets showed significant improvement in symptoms. This suggests that the "natural" path isn't about one specific magic food. It’s about the massive reduction in ultra-processed junk, emulsifiers like polysorbate 80, and carrageenan. These additives, common in "healthy" almond milks and protein bars, have been shown in lab studies to break down the mucus barrier in the gut. If you want an inflammatory bowel disease cure naturally, you have to stop eating the things that melt your gut’s protective coating.
The Stress Connection Is Not All In Your Head
It’s easy to get annoyed when someone says, "You just need to relax." IBD is an autoimmune condition, not a nervous breakdown. But the gut-brain axis is a two-way street. The Vagus nerve connects your emotional center directly to your intestines. When you are under chronic stress, your body releases cortisol. High cortisol increases gut permeability—often called "leaky gut."
Basically, if you’re stressed, your gut stays "open" to triggers.
Many people find that their "natural cure" involves things that have nothing to do with food. Mind-body interventions aren't just "woo-woo" anymore. A 2017 study published in Inflammatory Bowel Diseases journal found that patients who practiced MBSR (Mindfulness-Based Stress Reduction) had a significantly higher quality of life and lower perceived stress, which directly correlates to fewer flares. You can eat all the organic kale in the world, but if your nervous system is in "fight or flight" 24/7, your gut will stay inflamed.
Curcumin, Qat, and the Supplement Trap
Let's talk about supplements. Most of them are garbage. But a few have real weight behind them. Curcumin, the active compound in turmeric, is a heavy hitter. But here’s the catch: it’s notoriously hard for the body to absorb. If you're just shaking turmeric powder on your eggs, you aren't doing much for your IBD. You need a bioavailable form, often bound with phospholipids or black pepper extract.
Clinical trials have shown that curcumin, when used alongside standard treatments or as a standalone in mild cases, can help maintain remission in Ulcerative Colitis.
✨ Don't miss: How Long Before Bed to Take Magnesium: The Science of Getting It Right
Then there is Boswellia serrata (Indian frankincense). Some studies have suggested it can be as effective as mesalamine for certain patients. But you have to be careful. Taking a bunch of pills to "cure" a disease naturally can sometimes irritate the stomach lining even more. It's about precision, not volume.
The Hard Truth About Fiber
This is where it gets tricky. In the "natural health" world, everyone says "eat more fiber." In the IBD world, fiber can feel like swallowing glass during a flare.
There's a difference between soluble and insoluble fiber. Insoluble fiber (the "roughage" in kale and nut skins) acts like sandpaper on an inflamed colon. Soluble fiber (found in peeled carrots, oats, and squash) turns into a gel. This gel slows down transit time and actually helps the gut heal. If you are trying to manage your IBD naturally, you have to learn the nuances of food texture. Pureeing your vegetables might sound unappealing, but it's often the bridge between a flare and remission. It's about mechanical ease.
Vitamin D: The "Master Key"
If you haven't had your Vitamin D levels checked, do it tomorrow. Seriously. There is a massive correlation between low Vitamin D and IBD severity. Vitamin D isn't just a vitamin; it’s a pro-hormone that regulates the immune system. People with Crohn’s often have trouble absorbing fat-soluble vitamins, so they end up chronically deficient. This deficiency makes the immune system "twitchy."
Fixing your Vitamin D levels isn't a "cure," but it's often the foundation that allows other natural treatments to actually work. Most experts recommend keeping your levels in the higher end of the normal range—around 50-60 ng/mL—rather than just "not deficient."
Practical Steps for Natural Management
If you're serious about looking for an inflammatory bowel disease cure naturally, you need a systematic approach. You can't just try five different things at once and hope something sticks. You'll never know what actually worked.
- Start a "Food and Poop" Diary. It sounds gross, but it's your best diagnostic tool. Track what you eat and how your body reacts 2-24 hours later. You’ll start seeing patterns your doctor will never find.
- Eliminate the "Big Three" Emulsifiers. Check every label in your house for Carboxymethylcellulose (CMC), Polysorbate 80, and Carrageenan. Get rid of them. They are literal gut-shredders.
- Prioritize Sleep. Your gut lining regenerates while you sleep. If you're getting six hours of crappy sleep, you're denying your body the time it needs to fix the "leaks."
- Test, Don't Guess. Work with a functional medicine practitioner who can run a calprotectin test. This measures actual inflammation in your stool. If your calprotectin is high, your "natural" plan needs to be more aggressive. If it's low but you feel bad, you might be dealing with IBS on top of your IBD.
- Slowly Reintroduce. Once you find a "safe" diet (like the SCD or Autoimmune Protocol), don't stay in the restrictive phase forever. The goal is a diverse microbiome. Slowly add back one food at a time to see what your body can handle.
IBD is a complex, multi-factorial beast. It involves your genetics, your environment, your stress levels, and your diet. There is no magic pill—natural or pharmaceutical—that fixes it overnight. But by systematically removing triggers and adding in the building blocks for repair, many people find they can live a life where IBD is a background thought rather than a daily crisis. You have to be your own advocate. You have to be a scientist of your own body. It’s hard work, but for many, the reward of a quiet gut is worth every bit of the effort.
Focus on the Long Game
Don't get discouraged by a "bad day." Healing isn't linear. You might have three great weeks and then one day where your gut decides to revolt because of a stressful work meeting or a hidden ingredient in a restaurant meal. That doesn't mean you've failed or that "natural doesn't work." It just means your body is still calibrating. Stay the course, keep your Vitamin D up, and keep the processed chemicals out of your kitchen. Over time, those "bad days" usually get further and further apart until you realize you haven't thought about a bathroom in hours. That's the real win.