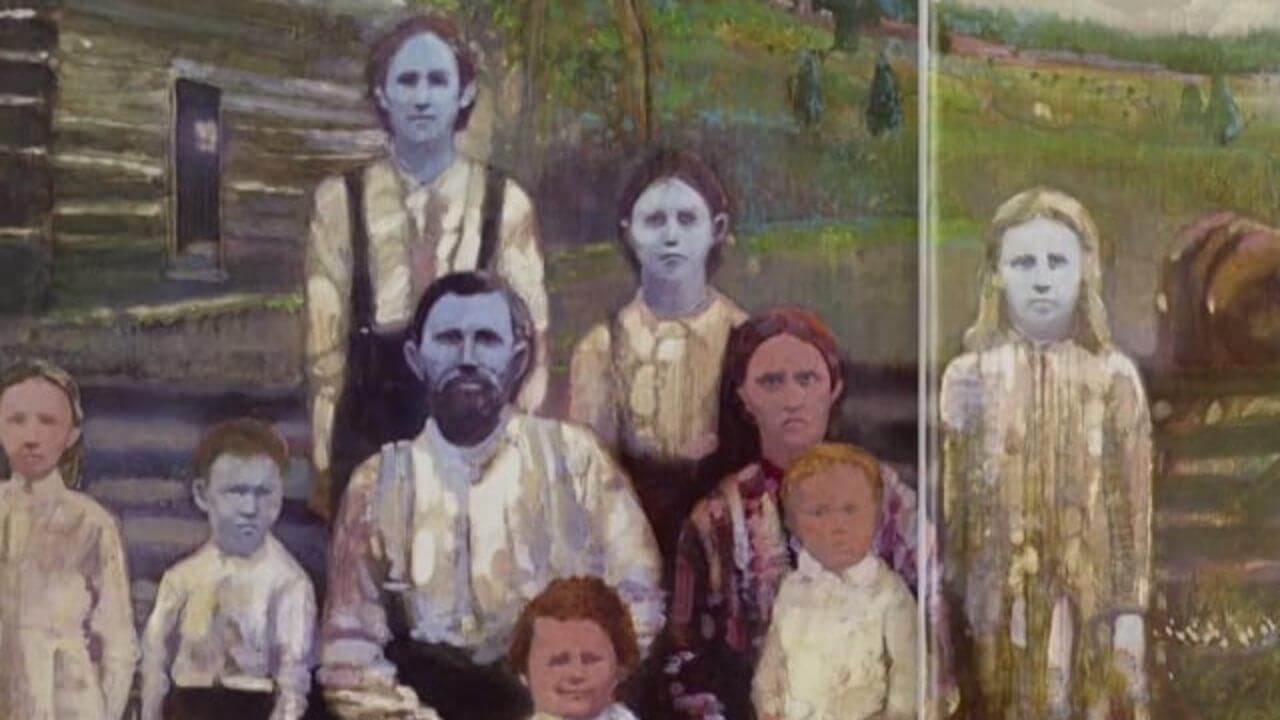
You’ve probably seen the photos. They look like a bad Photoshop job or maybe a leftover prop from a fantasy movie set. People with skin the color of a bruised plum or a clear summer sky. But the "Blue Fugates" of Troublesome Creek weren’t a hoax, and they weren't aliens. They were a real family living with a rare hereditary condition called methemoglobinemia. It’s a mouthful of a word, but basically, it’s a blood disorder that changes how your body carries oxygen. Honestly, the science behind it is just as fascinating as the folklore that grew up around it in the Appalachian hills.
When we talk about methemoglobinemia, we’re talking about a glitch in the hemoglobin. Hemoglobin is the protein in your red blood cells that hauls oxygen from your lungs to the rest of your body. Usually, it’s bright red, which gives our skin that pinkish, healthy glow. But sometimes, the iron in that hemoglobin shifts from a ferrous state to a ferric state. This "broken" version is called methemoglobin. It’s a darker, chocolate-brown color. It can’t carry oxygen effectively. If you have too much of it, your blood looks brown, and through your skin, that translates to a deep, startling blue.
👉 See also: Dance Exercise Routines Free: Why You Should Stop Paying for Cardio
Why the Fugate Family Turned Blue
The story starts in 1820. Martin Fugate, a French orphan, settled in the remote hills of eastern Kentucky. By a staggering stroke of genetic bad luck, he carried a recessive gene for a rare enzyme deficiency. He married Elizabeth Smith, who—against all statistical odds—also carried that same rare gene. Neither of them looked blue. They were just carriers. But when they had children, the "blue" trait emerged.
Because the area was so isolated, the gene pool stayed small. For over a century, the Fugates lived in the hollows, mostly keeping to themselves. They weren't sick, really. They lived long lives. They just looked like they’d been dipped in indigo. It wasn't until the 1960s that a hematologist named Madison Cawein decided to investigate the rumors of blue people in the mountains. He tracked down descendants like Patrick and Rachel Stacy and finally put a name to the condition.
The specific culprit was a lack of an enzyme called diaphorase (or cytochrome b5 reductase). Without this enzyme, the body can't convert methemoglobin back into the functional, red, oxygen-carrying hemoglobin. It stays stuck in that brown, useless state. The result? Cyanosis. The blue tint.
Is Methemoglobinemia Always Genetic?
No. That’s a huge misconception. While the Fugates are the famous face of the genetic version, most cases today are actually "acquired." This happens when certain chemicals or medications trick your blood into oxidizing.
Think about common stuff like benzocaine. It’s in those teething gels for babies and sprays used for sore throats. In some people, it triggers a massive spike in methemoglobin levels. Suddenly, you aren't getting enough oxygen to your tissues. Your lips turn blue. Your fingernails go dark. It’s terrifying because it happens fast. Other triggers include:
- Nitrates found in well water (often from fertilizer runoff).
- Certain antibiotics like dapsone.
- Inhaled nitrites (used recreationally or in industrial settings).
- Certain aniline dyes.
If you’re a healthy adult, your body usually keeps methemoglobin levels below $1%$. When those levels hit $10%$ to $20%$, you start looking "smurfy." If they climb toward $50%$, you’re looking at seizures, heart arrhythmias, and potential coma. It’s not just a skin color issue at that point; it’s a survival issue.
The Weirdest Cure You’ve Ever Heard Of
When Dr. Cawein met the Fugates, he tried something that sounds completely counterintuitive. He injected them with methylene blue. Yes, he used a blue dye to cure blue skin.
It sounds like a joke, but it’s high-level chemistry. Methylene blue acts as an electron donor that helps the body’s existing enzymes convert the brown methemoglobin back into red hemoglobin. The effect was almost instantaneous. Within minutes, the blue tint faded, and the Fugates saw their skin turn pink for the first time in their lives. They were given tablets to take daily to keep the enzyme process moving.
The Social Reality of the "Blue People"
Living blue wasn't easy, even if it wasn't physically painful. The Fugates were stigmatized. People in town whispered about them. They were called "The Blue People of Troublesome Creek," a name that stuck like a brand. It led to a lot of psychological isolation. They married within their own community not necessarily because they wanted to, but because they felt they had to.
Interestingly, as the 20th century progressed and the Appalachian region became more connected through better roads and migration, the "blue" gene started to thin out. When you marry someone from outside that specific genetic pocket, the chances of your kids being blue drop to almost zero. The last known "blue" descendant of the Fugates, Benjamin "Benjy" Stacy, was born in 1975. He was born dark blue, which panicked the doctors, but he eventually lost the tint as he grew older, only turning blue when he got cold or extremely angry.
What Science Tells Us Now
Today, we understand the molecular biology of methemoglobinemia much better. We know it’s usually an autosomal recessive condition. This means both parents have to be carriers. If only one parent has the gene, the kids will be totally normal-looking carriers.
There are also different types. Type I is mostly limited to the red blood cells, which is what the Fugates had. Type II is much more serious. It affects all tissues and can cause severe developmental delays and neurological issues because the enzyme is missing everywhere, not just in the blood. Fortunately, Type II is incredibly rare.
Real-World Precautions and Insights
If you’re worried about this, don’t be. Genetic methemoglobinemia is a medical unicorn. However, the acquired version is worth keeping on your radar.
📖 Related: The Real Limit: What's the Most Caffeine You Can Have in a Day?
- Check your well water. If you live in a rural area near farms, have your water tested for nitrates. This is the primary cause of "Blue Baby Syndrome." Infants are particularly vulnerable because their digestive systems haven't fully developed the ability to fight off the nitrites that form from nitrate-rich water.
- Be careful with numbing agents. Always follow the dosage on the back of benzocaine products. If you or a child suddenly looks pale or blue after using a topical anesthetic, it's a medical emergency. Don't wait.
- Know your history. If there is a history of unexplained "cyanosis" in your family, a simple blood test can check your diaphorase levels.
The story of the Fugates is a reminder that nature is weirder than fiction. It’s a story of isolation, chemistry, and a doctor who had the guts to inject blue dye into people who were already blue. It’s also a reminder that our health is often a delicate balance of enzymes we never even think about until they stop working.
If you suspect you've been exposed to an oxidizing agent, watch for "chocolate-colored" blood during a blood draw—it's the classic diagnostic sign. For those with the genetic trait, the treatment remains simple: avoid certain trigger drugs and, in some cases, maintain a regimen of Vitamin C or methylene blue as prescribed by a hematologist. Modern medicine has essentially turned a legendary mountain mystery into a manageable footnote in medical textbooks.
Actionable Next Steps
- Test your private well water annually for nitrates and nitrites, especially if you have infants in the house.
- Audit your medicine cabinet for benzocaine-based products; use them sparingly and never exceed the recommended frequency.
- Consult a hematologist if you experience persistent, unexplained bluish tint in your extremities that doesn't resolve with warmth, as this requires a differential diagnosis between methemoglobinemia and Raynaud’s phenomenon.