It happens faster than you think. You’re at a dinner party, you’ve got a nagging pain in your lower back, so you take a prescribed muscle relaxant. Then, someone pours a glass of Cabernet. It’s just one glass, right? Except your brain doesn't see it as "one plus one." When you combine CNS depressants and alcohol, the math is multiplicative, not additive. It’s not 1+1=2. It’s more like 1+1=5.
The results are often messy. Or worse, quiet.
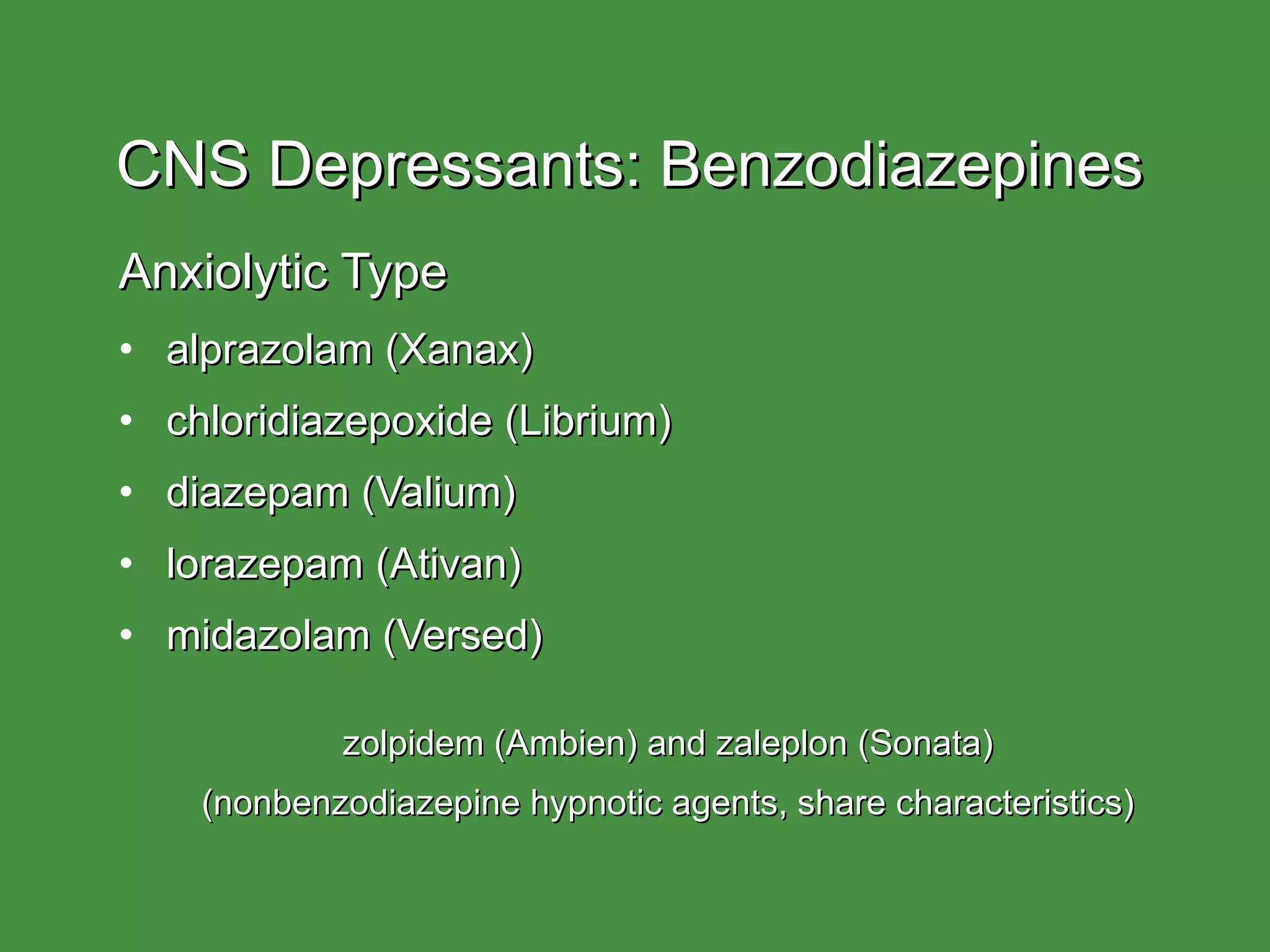
Central Nervous System (CNS) depressants are a massive category of drugs. We’re talking about benzodiazepines like Xanax or Valium, sleep aids like Ambien, and even those heavy-duty opioid painkillers. They all have one job: slow things down. They increase the activity of gamma-aminobutyric acid (GABA), a neurotransmitter that basically tells your neurons to "chill out." Alcohol does the exact same thing. When you throw both into your bloodstream simultaneously, you’re essentially slamming on the brakes of your respiratory system while driving downhill.
The Science of Synergistic Effects
Most people understand that getting "cross-faded" or mixing pills and booze makes you more drunk. But the biological reality is a bit more terrifying than just a bad hangover. This is what medical professionals call a synergistic effect.
Basically, the two substances amplify each other's potency.
If you take a dose of a sedative, your heart rate slows. Your breathing becomes shallower. Now, add alcohol. Ethanol is a small molecule that gets everywhere—it crosses the blood-brain barrier with ease. It hits the same GABA receptors that your medication is already hugging. This creates a "double-down" effect on the brainstem, which is the part of your brain responsible for the stuff you don't think about, like breathing and keeping your heart beating.
According to data from the Substance Abuse and Mental Health Services Administration (SAMHSA), alcohol is involved in roughly 18% of opioid-related emergency room visits and over 20% of benzodiazepine-related visits. It’s a leading factor in accidental overdoses because the "therapeutic window"—the gap between feeling relaxed and stopping breathing—shrinks to almost nothing.
Why Your Liver is Part of the Problem
Your liver is a workhorse, but it’s not a multitasker. It uses specific enzymes, primarily from the cytochrome P450 family, to break down toxins.
When you drink, your liver prioritizes the alcohol. It’s a literal poison, so the body wants it out immediately. While the liver is busy processing that margarita, the CNS depressants stay in your system longer than they’re supposed to. This leads to a toxic buildup. You might think the pill wore off three hours ago, but because your liver was distracted by the booze, the medication is still circulating at full strength.
The Different Players in the Game
Not all depressants are created equal, though they all share the same dangerous affinity for alcohol.
- Benzodiazepines (Benzos): These are the big ones—Xanax, Klonopin, Ativan. They are notoriously dangerous when mixed with alcohol. They both work on GABA-A receptors. The combination can lead to "blackout" states where you're technically awake but your brain has stopped recording memories.
- Sleep Medications: Ever heard of "Ambien eating" or "Ambien driving"? Z-drugs like zolpidem induce a hypnotic state. Alcohol turns that hypnotic state into a full-blown parasomnia where you might cook a three-course meal or get in a car and have zero recollection the next morning.
- Barbiturates: These aren't prescribed as much as they used to be because they are incredibly dangerous. Phenobarbital is one example. The line between a "calming dose" and a "lethal dose" is razor-thin, and alcohol erases that line entirely.
- Opioids: While technically analgesics, they heavily depress the CNS. Mixing OxyContin or Vicodin with alcohol is the primary cause of poly-substance overdose deaths in the United States.
What Real Impairment Looks Like
It isn't always someone falling over or slurring their words. Sometimes it’s subtle.
You might notice a "glassy" look in the eyes. Coordination goes out the window—not in a "stumbling drunk" way, but in a "missing the coaster with your drink" way. Paradoxically, some people get aggressive. This is called disinhibition. The part of your brain that says "maybe don't say that mean thing to your boss" is completely offline.
There's also the "nod." You see this a lot in emergency rooms. A patient will be talking, and then suddenly, their chin hits their chest. They're out. Seconds later, they bolt upright, unaware they even blinked. That is your brain struggling to stay conscious while its primary drive—the respiratory drive—is being suppressed.
💡 You might also like: What Disqualifies You From Donating Your Body To Science: The Real Reasons Programs Say No
The Myth of "Building a Tolerance"
"I've been on these meds for years, I can handle a beer."
Honestly? That’s the most dangerous sentence in pharmacology. While you might develop a psychological tolerance—meaning you don't feel as high—your brainstem never develops a tolerance to respiratory depression. Your "functional" level doesn't change the fact that your lungs are receiving fewer signals to expand.
Immediate Red Flags and What to Do
If you or someone you're with has mixed CNS depressants and alcohol, you need to watch for the "death rattle." It’s a labored, snoring-like sound. It isn't sleep. It’s the sound of an airway being partially obstructed because the muscles are too relaxed.
Other signs include:
- Blue or ashen lips and fingernails. (This is cyanosis—a lack of oxygen).
- Pinpoint pupils. (Common with opioids, though alcohol can sometimes mask this).
- Extremely slow pulse.
- Inability to be woken up by shouting or a sternum rub. (Take your knuckles and grind them hard into the center of their chest. If they don't flinch, call 911).
If you suspect an overdose, do not "let them sleep it off." That is how people die. Call emergency services. If opioids are involved, use Narcan (naloxone) if you have it. It won't hurt them even if opioids aren't the primary issue, and it could save their life if they are.
How to Stay Safe Without Being a Hermit
Look, life happens. You might be on an anti-anxiety med and want to toast at a wedding.
The safest answer is "don't do it." But if you are going to navigate this, you need to be smart. Talk to your pharmacist. Not just your doctor, but the pharmacist—they are the actual experts on drug-drug interactions. Ask them specifically about the half-life of your medication.
A drug like Valium has a incredibly long half-life (up to 100 hours). This means even if you didn't take a pill today, the pill you took two days ago is still in your blood waiting to party with that glass of wine.
Actionable Steps for Managing Your Health:
💡 You might also like: Mixing Bleach and Rubbing Alcohol: Why This "Cleaner" Is Actually a Death Trap
- Audit your cabinet: Look for the "Do Not Consume Alcohol" warning on your bottles. They aren't suggestions.
- The 24-Hour Rule: For many short-acting depressants, waiting a full 24 hours after your last dose before having a drink is a bare minimum, but this varies wildly by medication.
- Tell your "plus one": If you’re on these meds, make sure whoever you’re with knows. They need to know why you might be reacting strangely to a single drink.
- Use an interaction checker: Sites like Drugs.com have interaction checkers that can give you a baseline of the risks, though they don't replace a doctor's advice.
- Hydrate and eat: Food slows the absorption of alcohol, which can give your liver a fighting chance to handle things one at a time, though it doesn't eliminate the risk.
The reality is that the central nervous system is a delicate balance of electrical and chemical signals. Adding two different types of "downers" is playing chemistry with your life's essential functions. Stay informed, stay cautious, and never underestimate how much one pill can change the way your body processes a single drink.