Nursing school is a grind. You’re caffeine-deprived, staring at a care plan at 3 AM, and trying to figure out how to phrase a patient's breathing trouble without just saying "they can't breathe." That’s where the NANDA diagnosis list comes in. It’s basically the professional vocabulary for what nurses do every single day.
But honestly? It’s also a source of massive headaches.
NANDA-I (North American Nursing Diagnosis Association International) doesn't just hand out a static PDF and call it a day. They update this thing every three years. If you’re using a textbook from 2018, you’re probably using "outdated" language according to the latest 2021-2023 or the upcoming 2024-2026 cycles. This isn't just about semantics. It’s about clinical safety and getting paid. If the documentation doesn't match the approved taxonomy, the insurance companies get twitchy, and the hospital's data goes sideways.
The Real Deal on the NANDA Diagnosis List and Why It Changes
People think nursing is just following doctor's orders. Wrong. Doctors diagnose the disease—like "Pneumonia." Nurses diagnose the human response—like "Impaired Gas Exchange." That distinction is the entire reason the NANDA diagnosis list exists.
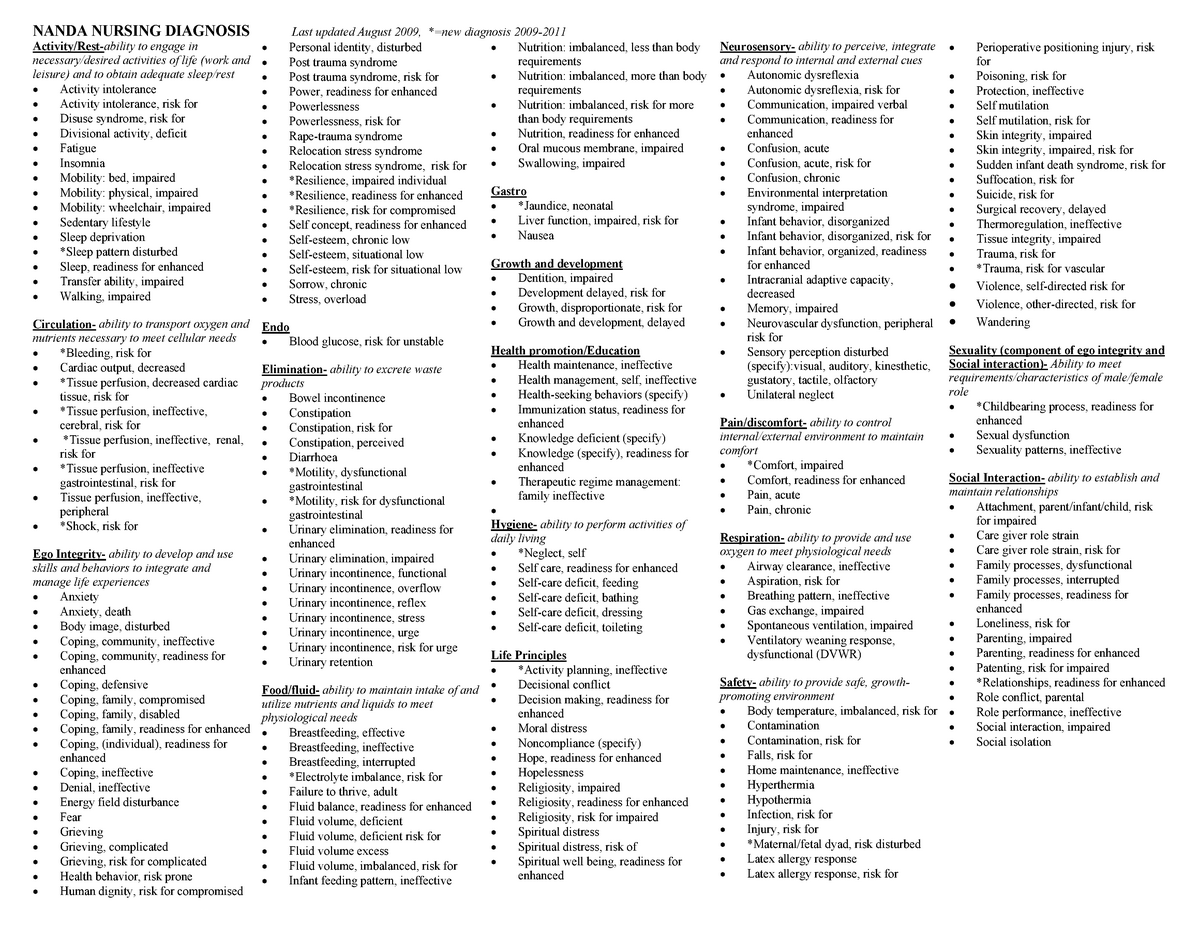
NANDA-I categorizes these into 13 domains. We're talking everything from Nutrition and Elimination to Perception/Cognition and Life Principles. It’s huge. There are over 250 diagnoses now. Some are "Problem-Focused" (what’s happening now), some are "Risk" (what might happen), and some are "Health Promotion" (making things even better).
Take "Risk for Falls." It’s a classic. Every floor nurse has written it a thousand times. But the nuances matter. Is it because of "Impaired Physical Mobility" or "Diminished Mental Status"? The NANDA list forces you to be specific.
Decoding the Structure: It’s Not Just a Name
Every entry on the NANDA diagnosis list follows a specific anatomy. You've got the Label (the name), the Definition (what it actually means), and the Defining Characteristics (the "signs and symptoms" or subjective/objective data).
If you don't have the "Defining Characteristics," you can't use the diagnosis. Period.
Let’s look at "Acute Pain."
Definition: Unpleasant sensory and emotional experience associated with actual or potential tissue damage.
If your patient says their pain is a 2/10 but they are laughing and eating, can you still use it? Technically yes, because pain is subjective. But if you look at the NANDA diagnosis list, you’ll see "protective behavior" or "expressive behavior" as characteristics. If those aren't there, maybe you should look at "Chronic Pain" or something else entirely.
The Most Common Diagnoses You’ll Actually Use
Most nurses live in about 20% of the total list. You aren't going to see "Spiritual Distress" on a post-op ortho floor as often as you see "Acute Pain" or "Impaired Skin Integrity."
- Impaired Gas Exchange: This is the big one for respiratory. It’s not just "short of breath." It’s about the O2 and CO2 exchange at the alveolar-capillary membrane.
- Deficient Fluid Volume: Dehydration. Whether it’s from a GI bug or a hemorrhage, this is a staple of the NANDA diagnosis list.
- Ineffective Coping: You see this a lot in Psych or Chronic Illness management. It’s when the patient’s internal resources just aren't cutting it.
- Risk for Infection: Basically every patient with an IV or an incision gets this one.
Nursing is messy. Sometimes a patient has five things going on at once. The NANDA list helps you prioritize. You deal with the "Impaired Gas Exchange" (Airway/Breathing) before you worry about "Readiness for Enhanced Knowledge."
The Shift Toward Precision
Recently, NANDA-I has been getting more "scientific." They’ve retired some old favorites that were too vague. They want "Evidence-Based."
For example, look at the "Sedentary Lifestyle" diagnosis. It’s gone. It was replaced and refined because "sedentary" didn't describe the clinical complexity enough. Now we look at things like "Inadequate Lifestyle Choice Management." It sounds like corporate speak, but it's meant to be more accurate for research.
How to Navigate the 13 Domains Without Losing Your Mind
The NANDA diagnosis list is organized into 13 "Domains." Think of them as folders on a computer.
👉 See also: Is female ejaculation real? The science behind what’s actually happening
- Health Promotion: Awareness of health and normalcy.
- Nutrition: Ingestion, digestion, absorption.
- Elimination and Exchange: Peeing, pooping, and breathing.
- Activity/Rest: Sleep, movement, cardiovascular stuff.
- Perception/Cognition: Thinking, sensing, paying attention.
- Self-Perception: Who am I? (Body image, self-esteem).
- Role Relationships: Being a parent, a worker, a friend.
- Sexuality: Identity and reproduction.
- Coping/Stress Tolerance: How they handle the bad stuff.
- Life Principles: Values and beliefs.
- Safety/Protection: Infection, falls, physical injury.
- Comfort: Pain (physical, social, environmental).
- Growth/Development: Are they hitting their milestones?
If you’re stuck on a care plan, don't just scroll the whole NANDA diagnosis list. Go to the domain. If your patient is confused, hit Domain 5. If they have a wound, hit Domain 11. It saves hours.
The Controversy: Why Some Nurses Hate the List
Ask a nurse with 30 years of experience about NANDA, and they might roll their eyes.
"I know what's wrong with the patient. Why do I need to find a specific phrase in a book to say it?"
It’s a valid gripe. The language can feel stiff. It can feel like it takes away from "real" nursing. But here’s the counter-argument: without a standardized NANDA diagnosis list, nursing isn't a "profession" in the eyes of academia or policy-makers. It’s just "caregiving." To have a science, you need a taxonomy. You need a way to measure outcomes.
If we all call "difficulty swallowing" something different, we can't track how well our interventions work across 1,000 different hospitals. NANDA provides the data.
The "PES" Format: The Secret Sauce
You can’t just pick a name from the NANDA diagnosis list and stop. You need the PES format.
P - Problem (The NANDA Label)
E - Etiology (The "Related To" factor)
S - Signs/Symptoms (The "As Evidenced By" factor)
Example: Impaired Physical Mobility (Problem) related to neuromuscular impairment (Etiology) as evidenced by inability to bear weight on right leg and 2/5 strength in lower extremities (Signs/Symptoms).
If you miss one of those three parts, your instructor or your auditor is going to have a field day.
Practical Steps for Mastering the NANDA Taxonomy
Don't try to memorize the whole thing. That’s a recipe for burnout. Instead, focus on the logic.
First, get the current edition. The Nursing Diagnoses: Definitions and Classification 2024-2026 is the gold standard. Anything older is just a historical document at this point.
Next, use "Cheat Sheets," but use them wisely. A lot of online "lists" are actually wrong or mix up NANDA with older systems like NIC (Nursing Interventions Classification) or NOC (Nursing Outcomes Classification). Remember: NANDA is the problem, NIC is the action, and NOC is the goal.
Finally, practice "Mapping." Take a real patient scenario.
"70-year-old male, post-hip replacement, refusing to use his walker because he’s afraid of falling, breathing slightly fast."
Look at the NANDA diagnosis list.
- Fear? Yes.
- Risk for Falls? Absolutely.
- Impaired Physical Mobility? Definitively.
- Ineffective Breathing Pattern? Maybe—need more data.
Actionable Next Steps:
- Check your sources: Verify if your hospital or school is using the 2021-2023 or 2024-2026 NANDA-I update.
- Download an app: There are several mobile versions of the NANDA diagnosis list that allow you to search by symptom. It’s much faster than flipping through a 500-page book at the nurse's station.
- Focus on the 'Related To' (R/T): Most errors in care planning happen because the "Related To" isn't something a nurse can actually treat. A nurse can't treat "Diabetes," but they can treat "Ineffective Health Management related to complexity of therapeutic regimen."
- Review the New Diagnoses: Every cycle, NANDA adds things like "Risk for Metabolic Syndrome" or "Disturbed Personal Identity." Staying current makes you look like the expert you are.
The NANDA diagnosis list isn't just a list of labels; it's the framework for how nurses think. Master the framework, and the paperwork stops being a chore and starts being a tool for better patient care. No more 3 AM meltdowns. Just solid, clinical reasoning.
Keep your assessment sharp. The data determines the diagnosis. If your assessment is weak, your NANDA choice will be too. Start with the patient, find the domain, and then let the taxonomy do the heavy lifting for your documentation.