You’re sitting on the couch, minding your own business, when you glance down at your wrist. Your Apple Watch or Fitbit buzzed. It says your heart rate is 58 beats per minute. Suddenly, you’re spiraling. Is that too low? Is it too high? Honestly, most people have no clue what a normal resting heart rate by age actually looks like because the "standard" range of 60 to 100 beats per minute (bpm) is kind of a massive oversimplification.
It’s a wide net. Too wide, maybe.
If you’re a 25-year-old marathon runner, 45 bpm might be perfectly healthy. If you’re 75 and sedentary, that same number could mean you’re headed for a pacemaker. Context is everything. Your heart isn't a metronome; it’s a living pump that reacts to every single thing you do, eat, or feel. Understanding the nuances of your pulse requires looking past the generic charts and digging into how age, sex, and fitness level collide to create your specific "normal."
The reality of normal resting heart rate by age
Let's get the big numbers out of the way first. For the vast majority of adults, the American Heart Association (AHA) sticks to that 60–100 bpm window. But that's like saying a "normal" height for a human is between four and seven feet. It’s technically true, but it doesn't tell you much about your health.
As we age, our heart's electrical system changes. The "pacemaker" cells in your sinoatrial node start to decrease in number. Fibrous tissue moves in. Basically, the heart's wiring gets a bit frayed. This doesn't necessarily mean your resting heart rate (RHR) climbs significantly as you get older; in fact, for many, it stays relatively stable or even dips slightly. However, your maximum heart rate definitely drops. That’s the real age-related shift.
Kids are a totally different story. A newborn’s heart is racing at 100 to 150 bpm. By age five, it’s closer to 70–110 bpm. By the time they hit those awkward teenage years, they finally settle into the adult range. If you see a toddler with a heart rate of 65 bpm, that's actually a reason to call a doctor, whereas for you, it’s the gold standard of cardiovascular fitness.
Breaking down the decades
Let’s look at how this typically tracks across the lifespan. In your 20s and 30s, your RHR is a massive indicator of your aerobic capacity. If you're active, you're likely seeing numbers in the high 50s or low 60s. By the time you hit your 40s and 50s, lifestyle choices—stress, caffeine, alcohol, and weight gain—start to pull that number upward.
🔗 Read more: Sunburn care at home: What actually works when you’re glowing like a lobster
- Infants (0-12 months): 100–160 bpm. Their little hearts have to work overtime to support rapid growth.
- Children (1-10 years): 70–120 bpm.
- Teens and Adults (11+): 60–100 bpm.
- Elite Athletes: 40–60 bpm. This is where things get interesting.
Why do athletes have such low rates? Efficiency. Their heart muscle is so strong that it can pump a massive volume of blood with a single squeeze. It doesn't have to beat as often. If you aren't an athlete and your heart rate is 42, that’s called bradycardia, and it might be why you feel dizzy when you stand up.
Why the "60 to 100" range is being challenged
Recent research suggests that 100 bpm is actually too high for a "normal" resting ceiling. A study published in the Journal of the American College of Cardiology suggested that individuals with a resting heart rate at the higher end of the normal range—specifically above 80 bpm—might have a higher risk of cardiovascular issues over time compared to those in the 60s.
Think about it this way. If your heart beats 85 times a minute versus 65 times a minute, that’s 20 extra beats every minute. In an hour, that’s 1,200 extra beats. In a day? Nearly 29,000 extra thumps. Over a decade, that's a lot of extra wear and tear on your valves and arteries.
Dr. Sharonne Hayes from the Mayo Clinic often points out that while 90 bpm is technically "normal," it might be a sign that your body is under systemic stress. Maybe it’s chronic inflammation. Maybe it’s poor sleep. Or maybe you're just incredibly dehydrated. Your RHR is basically a "check engine" light. It doesn't tell you exactly what’s wrong, but it tells you that something is up.
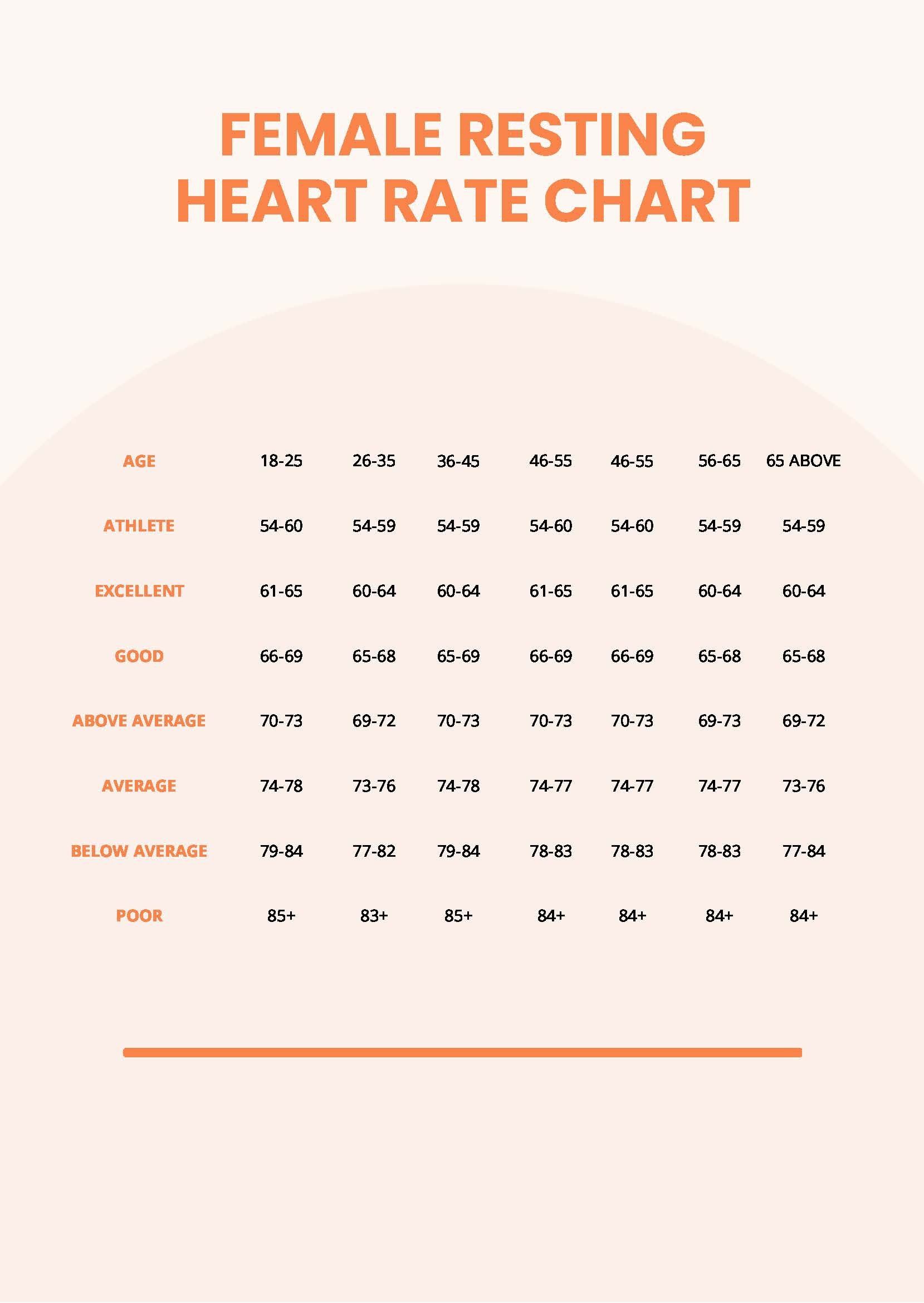
The Sex Gap: Men vs. Women
Women generally have higher resting heart rates than men. It’s not a fitness thing; it’s a size thing. Because women typically have smaller hearts, the organ has to beat more frequently to move the same amount of blood. Pregnancy also throws a wrench in the numbers. During pregnancy, blood volume increases by up to 50%, which means the heart has to pump faster just to keep up. It’s not unusual for a pregnant woman’s RHR to jump by 10 or 15 beats per minute.
Variables that mess with your numbers
You cannot just take your pulse once and decide you're healthy. That's a mistake. So many things can temporarily spike your normal resting heart rate by age that it’s almost funny.
- The "White Coat" Effect: Your heart rate at the doctor's office is almost always higher than at home. Anxiety is a powerful stimulant.
- Temperature: When it’s hot, your heart pumps more blood to the surface of your skin to help you cool down. Your pulse will climb.
- Dehydration: Less fluid in your veins means your blood is thicker and harder to move. The heart compensates by speeding up.
- Medications: Beta-blockers will tank your heart rate (on purpose), while some asthma inhalers or ADHD meds can send it through the roof.
I once worked with a guy who was terrified because his RHR was 95. Turns out, he was drinking four double espressos before 10:00 AM. We cut the coffee, and his heart rate "miraculously" dropped to 72 within a week. Sometimes the answer isn't a medical condition; it’s just your morning routine.
How to measure it accurately
Stop checking your heart rate at 2:00 PM after a stressful meeting. That’s useless data. The only time to find your true resting heart rate is the moment you wake up, before you even get out of bed. Don't check it after you've scrolled through Instagram for twenty minutes and gotten annoyed by a political post. Wake up, find your pulse on your wrist or neck, and count for 60 seconds. Do this for three days in a row and take the average. That is your baseline.
When should you actually worry?
Consistency matters more than the specific number. If you’ve always been a 65 bpm person and suddenly you’re sitting at 85 bpm for no apparent reason, that’s worth a conversation with a professional.
Tachycardia (over 100 bpm at rest) can lead to blood clots, heart failure, or fainting spells if left untreated. On the flip side, bradycardia (under 60 bpm) is only a problem if it comes with symptoms. If you’re at 52 bpm but you feel energetic and sharp, you’re probably fine. If you’re at 52 bpm and you feel like you’re walking through molasses and can't focus, your brain might not be getting enough oxygenated blood.
The role of Heart Rate Variability (HRV)
If you want to be a real nerd about this, look at HRV. While RHR is the average number of beats, HRV looks at the tiny fluctuations in time between each beat. A high HRV usually means your nervous system is balanced and you're recovering well. A low HRV—even if your RHR looks "normal"—can be a sign of overtraining or impending illness. Many athletes now use HRV more than RHR to decide if they should hit the gym hard or take a rest day.
🔗 Read more: Regency at Whitmore Lake: What Most People Get Wrong
Actionable steps to optimize your heart rate
You aren't stuck with the heart rate you have today. The heart is a muscle. You can train it.
- Prioritize Zone 2 Cardio: This is "easy" cardio where you can still hold a conversation. Think brisk walking or light cycling. Doing this for 150 minutes a week strengthens the heart's stroke volume, which naturally lowers your RHR over time.
- Manage Magnesium: This mineral is crucial for electrical signaling in the heart. Many people are deficient, which can lead to palpitations or a slightly elevated pulse. Focus on spinach, almonds, and pumpkin seeds.
- Sleep Hygiene: One night of bad sleep can spike your RHR by 5–10 beats the next day. Your heart needs that downtime to repair.
- Alcohol Cessation: Alcohol is a cardiac stimulant in the short term and a depressant in the long term. Even one glass of wine can raise your resting heart rate for several hours during sleep, preventing deep recovery.
The goal isn't necessarily to have the lowest heart rate in the world. It’s to have a heart that is resilient. A heart that can jump to 150 bpm when you’re running for the bus and settle back down to 65 bpm within minutes of sitting down. That recovery speed—how fast you return to your "normal"—is often a better indicator of health than the resting number itself.
Keep an eye on the trends, not the daily blips. If the trend is moving toward the 60s and 70s, you're likely on the right track for long-term cardiovascular longevity. If you notice persistent chest pain, shortness of breath, or palpitations that feel like a "flopping fish" in your chest, skip the Google search and get an EKG. Real data from a medical professional beats a wrist-worn sensor every single time.
Check your pulse tomorrow morning. Start there. Note the number, then look at your lifestyle. Small tweaks to your hydration and movement can move the needle faster than you might think. Your heart is literally doing the heavy lifting for your entire life; the least you can do is give it the right conditions to work a little less hard.