Ever sat perfectly still and felt your heart thumping against your ribs like a trapped bird? It’s unnerving. You check your smartwatch. It says 82. Then 74. Then 88. You start wondering if you’re dying or just caffeinated. Most people think normal resting heart rates are a static number, like a height or a shoe size, but honestly, that’s just not how biology works. Your heart is a reactive engine.
Most doctors will tell you the standard range is 60 to 100 beats per minute (bpm). That’s the classic textbook answer from the American Heart Association. But if you’re a marathon runner and your heart is hitting 95 while you’re watching Netflix, something is probably wrong. Conversely, if you're a sedentary office worker and your heart rate is 42, you might be heading for a fainting spell. Context is everything.
The 60 to 100 Myth
We've been taught that anything under 100 is "fine." That's a bit of a stretch. Recent data, including a massive study published in The Lancet, suggests that consistently sitting at the higher end of that "normal" range—say, 80 to 90 bpm—actually correlates with a higher risk of cardiovascular issues over a ten-year period. It’s not that 85 bpm is "sick," but it might be a sign that your heart is working harder than it needs to.
Why the 60–100 range? It’s a wide net. It’s designed to catch the extremes. If you’re at 110 (tachycardia) or 40 (bradycardia), it triggers a clinical red flag. But the "sweet spot" for most healthy adults usually hovers between 50 and 70 bpm.
Think about it this way. If your heart beats 80 times a minute instead of 60, that’s an extra 28,800 beats per day. Over a year, that’s over 10 million extra beats. That is a lot of unnecessary wear and tear on your heart muscle and your arteries.
What actually shifts the needle?
Your heart rate is basically a real-time report card of your nervous system.
If you didn't sleep well last night, your sympathetic nervous system (your "fight or flight" mode) stays slightly engaged. Your heart rate climbs. Dehydration is another big one. When you're low on fluids, your blood volume drops. To keep your blood pressure stable and move oxygen around, your heart has to pump faster. It’s simple physics.
Then there’s the "White Coat Effect." Many people get a reading of 95 at the doctor's office because they’re stressed about being there, even though they’re a cool 65 at home. This is why a single snapshot of your normal resting heart rates is almost useless. You need a trend.
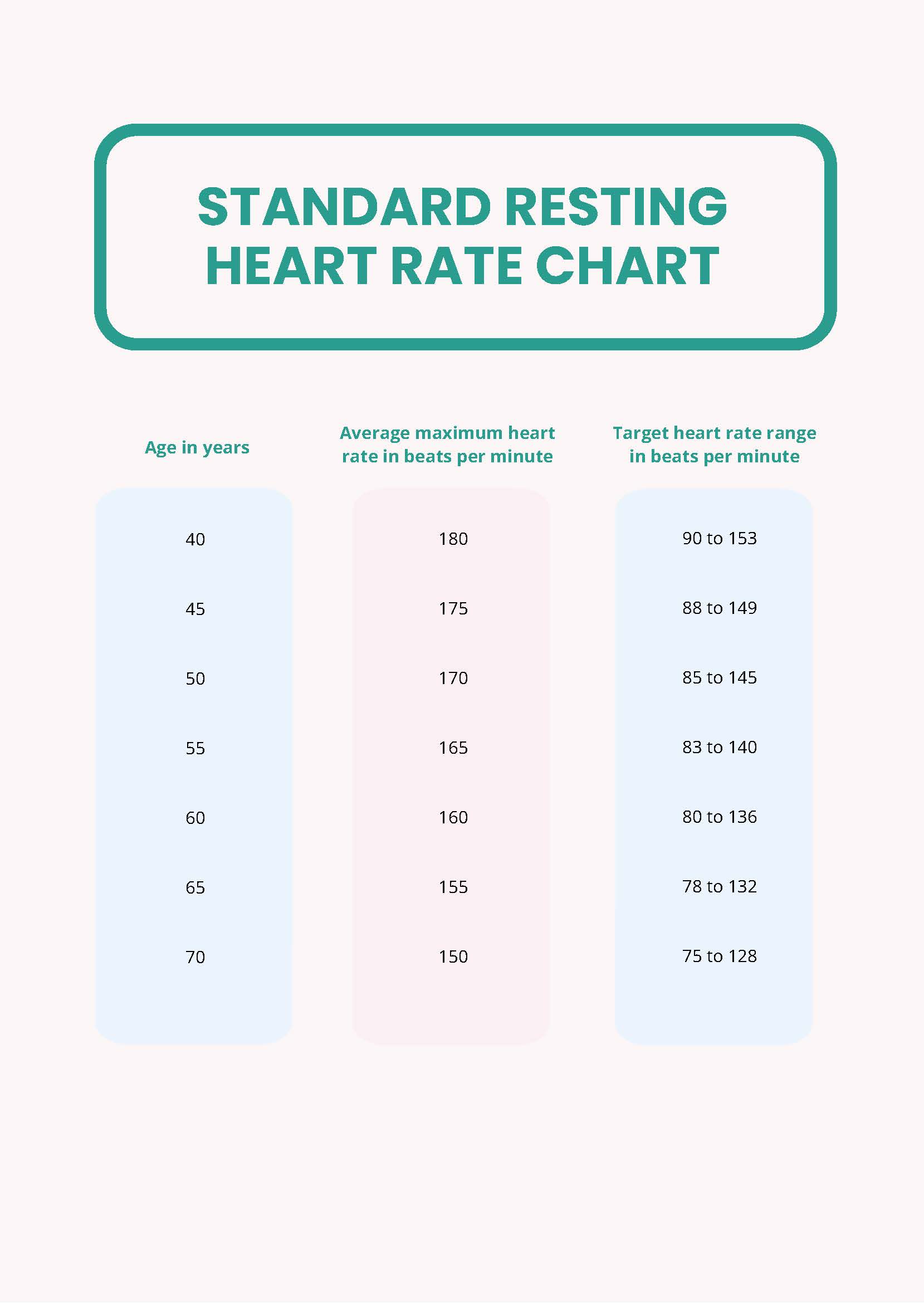
- Age: Kids have much higher rates. A newborn might sit at 130 bpm. As we age, it slows down, though the "normal" adult range stays relatively flat until seniors might see a slight increase again.
- Fitness: This is the most famous variable. Athletes like Miguel Induráin, the legendary cyclist, reportedly had a resting heart rate of 28 bpm. For a normal person, that’s a medical emergency. For him, it was a sign of a massive, hyper-efficient heart.
- Temperature: If it’s 95 degrees out and humid, your heart has to work harder to radiate heat away from your skin.
- Emotions: Anxiety isn't just "in your head." It’s a chemical cascade of adrenaline and cortisol that physically forces the sinoatrial node—your heart's natural pacemaker—to fire faster.
The problem with your smartwatch
Apple Watches, Garmins, and Fitbits are great, but they’ve turned us all into hypochondriacs. These devices use photoplethysmography (PPG). Basically, they flash green LED lights into your skin to measure blood flow. It’s surprisingly accurate, but it’s not perfect.
If the band is loose, or if you have certain skin tones or tattoos, the reading can skip. People often see a "spike" to 140 while they’re washing dishes and panic. Usually, that’s just a "noise" error in the sensor.
The most accurate way to find your normal resting heart rates is still the old-school way. First thing in the morning. Before you get out of bed. Before you check your email. Two fingers on the radial artery (your wrist) or the carotid (your neck). Count for 60 seconds. Do this for three days and average it. That is your true baseline.
When should you actually worry?
Usually, a high heart rate is a symptom, not the disease itself. If you're consistently seeing numbers over 100, it could be thyroid issues (hyperthyroidism), anemia, or even a lingering low-grade infection.
But there are specific "red flag" pairings.
If a high or low heart rate comes with chest pain, shortness of breath, or lightheadedness, the number doesn't matter anymore—the symptoms do. Shortness of breath is the big one. If your heart is racing and you can't catch your breath while sitting on the couch, that's not "stress." That's a "call the doctor" moment.
💡 You might also like: Testicular Health: Why Your Balls in a Sack Deserve Better Care
We also have to talk about "Heart Rate Variability" or HRV. This is the variation in time between each heartbeat. Interestingly, you actually want this to be high. A heart that beats exactly like a metronome (low HRV) is often a sign of a stressed, rigid nervous system. A heart that fluctuates slightly is a sign of a healthy, resilient body.
Practical steps for a better baseline
Lowering a high resting heart rate isn't some mystical art. It’s mostly about boring, consistent habits.
- Cardio, but not too much. Zone 2 training—walking fast enough that you can still talk but would rather not—is the gold standard for strengthening the heart muscle. It makes the heart "stretchy" and increases the amount of blood pumped per beat (stroke volume).
- Magnesium and Potassium. Your heart is an electrochemical pump. If your electrolytes are off, the "electrical" part of that pump gets twitchy. Most people are chronically low on magnesium.
- The Breath. You can manually override your heart rate. It’s the only part of the autonomic nervous system you can control. Long, slow exhales stimulate the vagus nerve, which tells your heart to slow down. If you're at 85, five minutes of "box breathing" can often drop you into the 70s.
- Alcohol. Sorry, but that glass of wine at night wreaks havoc on your heart rate while you sleep. It’s a toxin that the body has to process, which keeps your metabolism—and your heart—running hot all night.
The bottom line on your pulse
Don't obsess over a single number. Your heart rate is a conversation between your brain and your environment. If it's a bit high today, maybe you just need a glass of water and a nap.
If you’re concerned, start a simple log. Write down your morning pulse, your caffeine intake, and how you felt that day. After two weeks, you'll have more useful data for your doctor than a thousand frantic Google searches could ever provide.
Actionable Next Steps
- Establish your baseline: Measure your pulse manually for three consecutive mornings before getting out of bed to find your true "resting" state.
- Audit your stimulants: If your rate is consistently over 85, track your caffeine and nicotine intake for 48 hours to see if there is a direct correlation.
- Hydration Test: Drink 16 ounces of water and re-measure your heart rate 30 minutes later; a significant drop often indicates chronic mild dehydration.
- Check your medications: Review any over-the-counter decongestants or prescriptions with a pharmacist, as many common drugs (like asthma inhalers or ADHD meds) naturally elevate the heart rate.