You’re sitting on the couch, maybe scrolling through your phone, and you feel that familiar rhythmic thumping in your chest. Or maybe you don't feel it at all, but your Apple Watch just buzzed to tell you your regular resting heart rate dipped below 50 while you were napping. Suddenly, you're spiraling. Is that good? Is it a sign of an elite athlete's engine, or is your heart actually failing? Honestly, most of us have no clue what those numbers really mean because we’ve been fed a diet of overly simplified "averages" that don't account for the messy reality of human biology.
It’s complicated.
Your heart isn't a metronome. It’s a dynamic muscle that reacts to everything from the double espresso you drank three hours ago to the fact that you’re slightly dehydrated because it’s Tuesday and you forgot to drink water. When we talk about a regular resting heart rate, we're usually looking for that sweet spot where the heart is pumping the least amount of blood possible because you’re at total rest. For most adults, that’s traditionally been cited as 60 to 100 beats per minute (bpm). But if you ask a cardiologist today, they’ll tell you that "normal" is a sliding scale.
Why the 60 to 100 Range is Kinda Dated
We’ve stuck with the 60–100 bpm range for decades. It’s the standard. However, many experts, including those at Harvard Health, suggest that a resting rate on the lower end of that spectrum—or even slightly below it—is often a sign of better cardiovascular fitness. If your heart is efficient, it doesn't need to beat as often to move blood through your system. It’s like a high-performance engine idling at low RPMs.
Think about it this way.
A person with a resting rate of 85 bpm is technically "normal." But recent longitudinal studies, like those published in the journal Heart, have shown that people with resting heart rates at the higher end of the 60–100 range actually face a higher risk of cardiovascular issues over time compared to those sitting in the 50s or 60s. So, while 90 bpm won't land you in the ER today, it might be a nudge from your body saying it's working harder than it needs to.
📖 Related: Standing Stomach Crunches: Why Your Core Routine is Probably Missing This
The Athlete’s Curve
If you’re a marathon runner or a cyclist, your regular resting heart rate might be 40 bpm. For a sedentary person, that number (bradycardia) might cause fainting or dizziness. For an athlete, it’s just efficiency. This is where the context of your lifestyle matters more than the raw data on your wrist.
The Stealth Killers of Your Heart Rhythm
Stress is the obvious one. We all know that. But there are weirder things that mess with your baseline. Take temperature, for instance. When it’s sweltering outside, your body shunts blood to the skin to help you cool down. Your heart has to beat faster to maintain your blood pressure while doing this. Suddenly, your "resting" rate is up by 10 beats, and you're wondering if you’re getting sick.
You aren't. You're just hot.
Then there’s the "White Coat Effect." Many people walk into a doctor’s office, see the stethoscope, and their heart rate jumps. This makes getting an accurate reading of a regular resting heart rate in a clinical setting surprisingly difficult. This is why many physicians now prefer data from wearable devices or home monitoring, provided the patient knows how to take a proper reading.
To get a real number, you need to be still. Not "just sat down" still. I mean five minutes of silence. No phone. No talking. No caffeine in the last hour. If you check your pulse right after a stressful email, you aren't measuring your resting rate; you’re measuring your reaction to your boss.
🔗 Read more: I Got Some Pressure Built Up: Why Your Body Feels Like a Ticking Clock
Genetics and the Biological Lottery
We don't talk enough about the fact that some people are just wired "fast" or "slow."
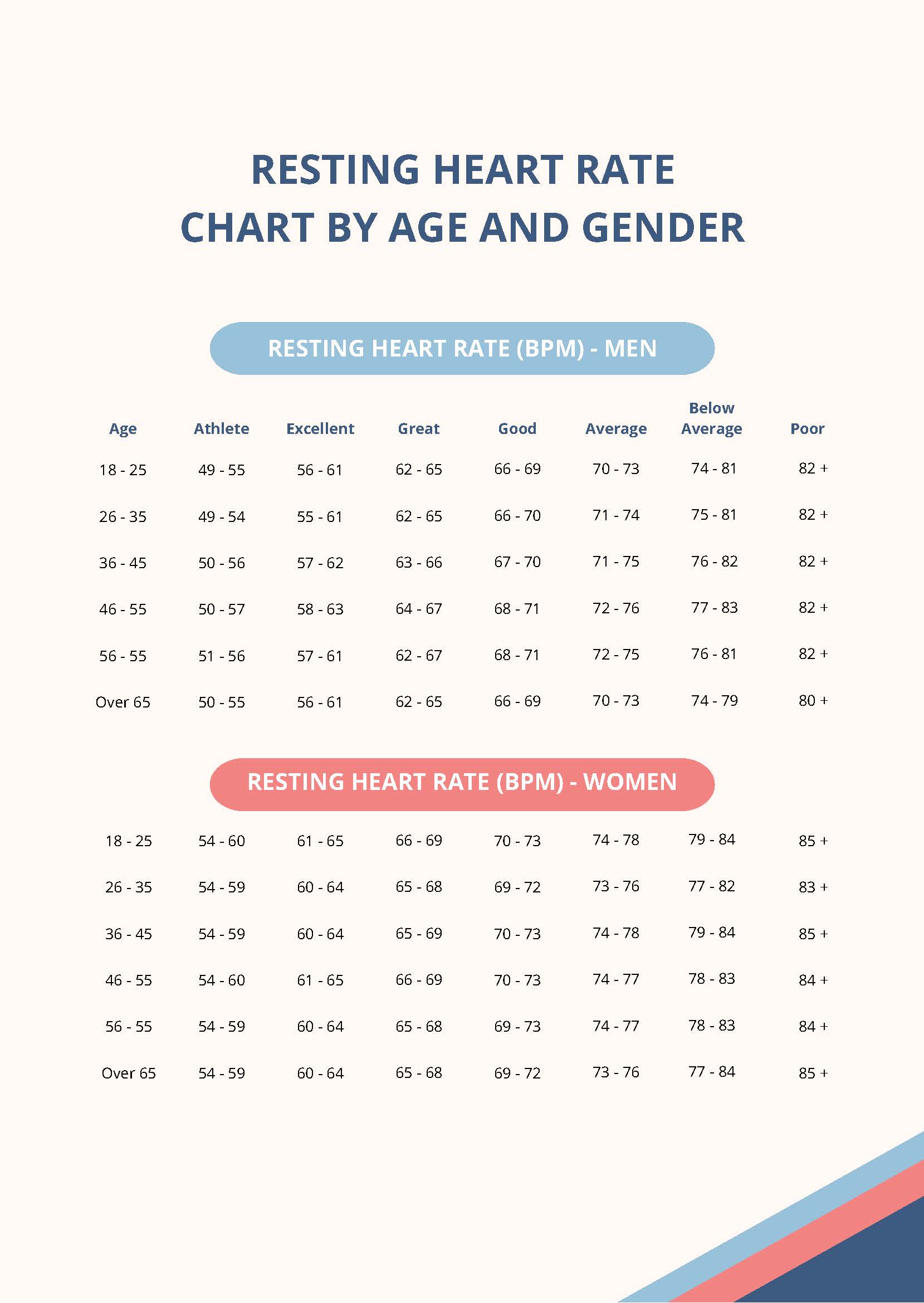
Age plays a massive role, too. In children, a "normal" resting heart rate is much higher—sometimes over 100 bpm for toddlers—because their bodies are smaller and their hearts beat faster to keep up with rapid metabolic demands. As we age, the heart's electrical system can undergo fibrosis or natural wear and tear, which sometimes slows the rate down or, conversely, leads to arrhythmias like Atrial Fibrillation (AFib).
- Beta-blockers: These meds are designed to slow the heart down.
- Thyroid issues: An overactive thyroid (hyperthyroidism) can send your heart racing, while an underactive one can make it sluggish.
- Anemia: When you don't have enough red blood cells to carry oxygen, your heart has to pump faster to compensate. It’s exhausting.
When Should You Actually Worry?
Numbers are just data points until they’re paired with symptoms. A regular resting heart rate of 110 (tachycardia) is a problem if it stays there while you’re watching Netflix. If it’s accompanied by chest pain, shortness of breath, or a feeling that your heart is "flopping" like a fish in your chest, that’s the time to call a professional.
Dr. Sahil Parikh from Columbia University Irving Medical Center notes that the trend is often more important than a single reading. If you’ve spent five years at 65 bpm and suddenly you’re consistently at 85 bpm, something has changed. Maybe it’s stress. Maybe it’s a new medication. Or maybe your heart is struggling with an underlying issue you haven't noticed yet.
The Role of Sleep
Your heart rate should drop significantly while you sleep. This is the "dipping" phenomenon. If your heart rate stays high throughout the night, it’s often a sign of Sleep Apnea or extreme chronic stress. Your heart never gets its "break," which can lead to long-term wear.
How to Actually Lower a High Resting Rate
You can’t just wish your heart rate lower. It takes consistent effort, but the heart is remarkably plastic. It adapts.
- Zone 2 Cardio: This is the magic "low and slow" exercise. It’s jogging or walking at a pace where you can still hold a conversation. It strengthens the heart muscle, allowing it to pump more blood per beat.
- Magnesium and Hydration: Electrolyte imbalances are a common, and easily fixable, cause of heart palpitations and elevated rates.
- Vagus Nerve Stimulation: Techniques like deep diaphragmatic breathing or even splashing cold water on your face can trigger the parasympathetic nervous system, which acts as the "brake" for your heart.
It’s worth noting that "overtraining" is a real thing. If you’re a gym rat and you notice your regular resting heart rate has jumped by 5–10 beats over several days, you’re likely not recovering. Your heart is literally telling you to take a day off. Listen to it.
The Wearable Trap
We live in an era of "Overshare" from our gadgets. I’ve seen people get genuine anxiety because their watch told them their heart rate variability (HRV) was low or their resting rate was "off" by three beats.
🔗 Read more: I accidentally ate moldy bread: Here is what actually happens to your body
Don't let the data drive you crazy.
Consumer wearables are great for trends, but they aren't medical-grade ECGs. They can be fooled by a loose watch strap or a dark tattoo on your wrist. Use the data as a guide, not a gospel. If the watch says something weird, check your pulse manually. Two fingers on the radial artery (the thumb side of your wrist), count for 15 seconds, multiply by four. It’s the old-school way, and it still works.
Moving Forward With Your Data
Understanding your regular resting heart rate is basically about learning the language of your own body. It’s a baseline. Once you know what yours is—whether it’s 58 or 72—you can spot the deviations that actually matter.
Actionable Steps for Better Heart Health
- Establish a Baseline: Measure your heart rate manually for three consecutive mornings before you get out of bed. Average these three numbers to find your true "rested" baseline.
- Check Your Meds: Review any over-the-counter supplements or prescriptions with your pharmacist. Things as simple as decongestants can spike your heart rate for hours.
- Prioritize Sleep Hygiene: Aim for a "dipping" heart rate by avoiding alcohol and heavy meals within three hours of bedtime. Alcohol is a massive heart rate stimulant that lasts long after the "buzz" wears off.
- Incorporate Interval Training: While Zone 2 is great for efficiency, short bursts of high-intensity interval training (HIIT) can improve the heart's ability to recover quickly from stress.
- Consult a Professional if Needed: If your resting rate is consistently over 100 or under 50 (and you aren't an athlete), schedule an EKG. It’s a simple, non-invasive test that provides a clear picture of the heart's electrical activity.
The goal isn't to have the "perfect" number. The goal is to have a heart that responds well to the demands of your life and returns to a calm, steady state when those demands are over. Pay attention to the trends, ignore the minor daily fluctuations, and treat your heart like the high-performance machine it is.