Finding out your blood type is "negative" while you’re staring at a positive pregnancy test can feel like a punch in the gut. You’ve probably heard whispers about "blue babies" or the body attacking the fetus, and honestly, that sounds like something out of a medical thriller. But here’s the reality. It’s manageable. In fact, it’s one of the greatest success stories in modern obstetrics. If you have an rh factor negative pregnancy, you aren't "broken" or "incompatible" with your baby. You just have a specific biological quirk that requires a little bit of proactive timing and a couple of shots.
Most people don't think about their blood type until they're forced to. You’re either A, B, AB, or O. Then there’s that little plus or minus sign. That sign is the Rhesus (Rh) factor, a protein found on the surface of red blood cells. If you have it, you're Rh-positive. If you don't? You're Rh-negative. It’s an inherited trait, much like eye color or height. About 15% of Caucasians, 8% of African Americans, and only about 1% of Asians are Rh-negative.
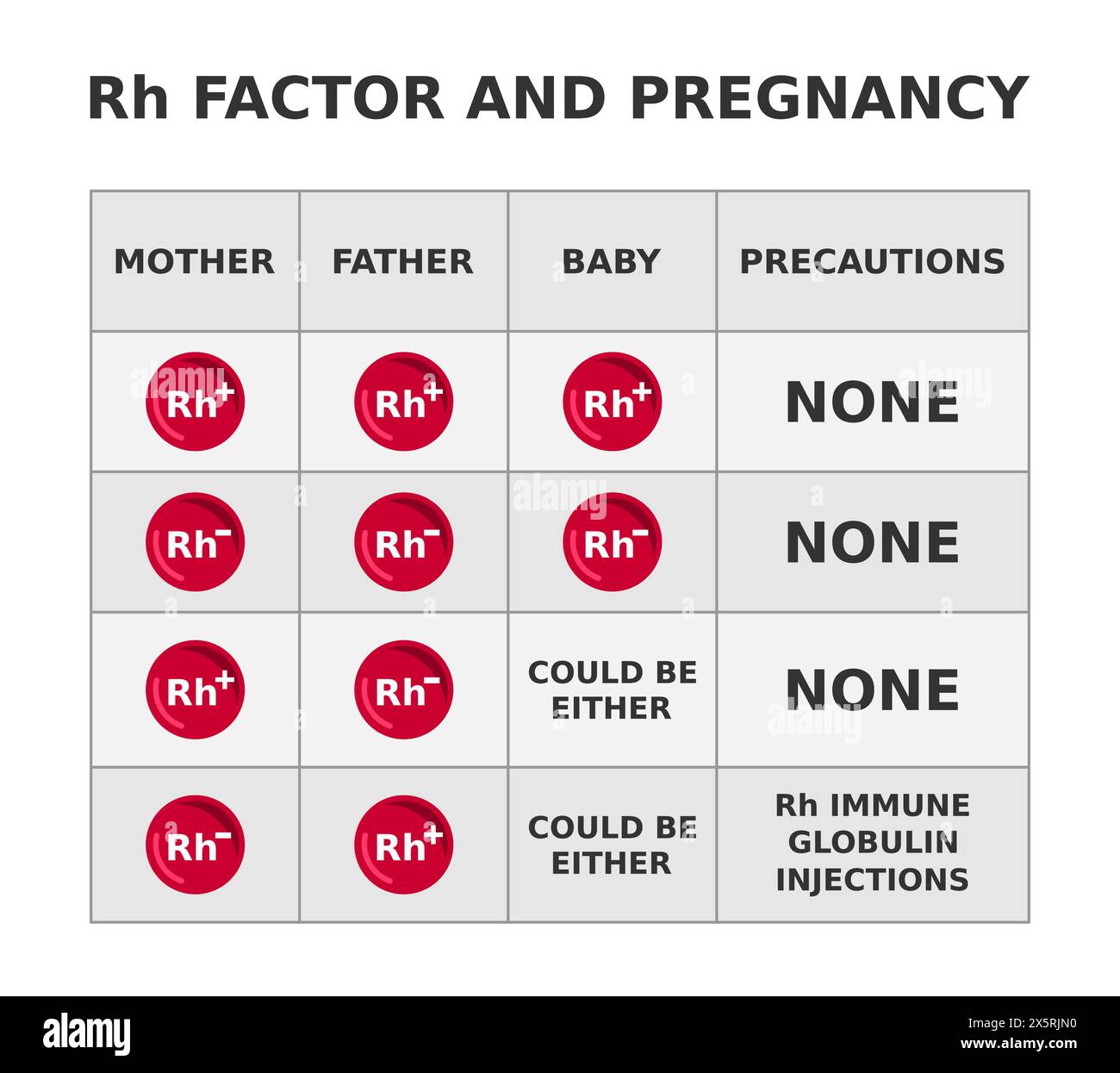
The "problem" only shows up if the person carrying the baby is Rh-negative and the biological father is Rh-positive. If the baby inherits that positive blood type, your immune system might see the baby’s blood as a foreign invader. It’s sort of like how your body reacts to a virus. It builds an army.
Why Rh Factor Negative Pregnancy Matters for Your Second Baby
Here is the weird part: your first pregnancy is usually totally fine.
During a typical pregnancy, your blood and the baby’s blood don’t actually mix. The placenta acts like a high-security border. But during birth, or if you have a miscarriage, an abdominal injury, or an invasive test like an amniocentesis, some of the baby’s Rh-positive blood can slip into your system. Your body looks at those Rh proteins and says, "Wait, that shouldn't be here." It starts producing antibodies. This process is called sensitization.
Once you are sensitized, your body "remembers" how to make those antibodies forever.
If you get pregnant again with another Rh-positive baby, those antibodies are already primed. They are small enough to cross the placenta. They find the baby’s red blood cells and begin destroying them. This leads to Hemolytic Disease of the Fetus and Newborn (HDFN). In the old days, this was often fatal or led to severe brain damage. Today? We have Rh immune globulin, better known by the brand name RhoGAM.
The RhoGAM Revolution
Before RhoGAM was introduced in 1968, thousands of babies died every year from Rh disease. It was a localized epidemic that doctors couldn't solve. Then researchers discovered that if you inject an Rh-negative mother with Rh antibodies (the "shot"), it basically tricks the immune system. It cleans up any stray Rh-positive fetal cells before the mother's immune system even notices them.
It’s essentially a temporary shield.
You usually get this shot around week 28 of your pregnancy. Why then? Because that’s when the "leakage" between mother and baby is most likely to start as the placenta ages. You’ll get another shot within 72 hours after delivery if the baby is confirmed to be Rh-positive. If the baby turns out to be Rh-negative like you? No second shot needed.
👉 See also: How Do I Do a Push Up? Why Your Form Is Probably Failing You
I’ve talked to women who felt guilty about needing medical intervention. Don't. It’s just chemistry.
Real World Scenarios and Misconceptions
People get really confused about the "father's role" in this. If the father is also Rh-negative, there is zero risk. Two Rh-negative parents cannot produce an Rh-positive child. Period. The genetics don't allow for it. However, if the father is Rh-positive, he might carry one "negative" gene and one "positive" gene (heterozygous), or two "positive" genes (homozygous). If he's homozygous, every single baby you have will be Rh-positive. If he's heterozygous, it's a 50/50 coin flip every time.
What happens if you miss the shot?
If you become sensitized, RhoGAM won't help you anymore. It’s a preventative, not a cure. If you already have the antibodies, your pregnancy becomes "high risk." You’ll be seeing a Maternal-Fetal Medicine (MFM) specialist. They’ll use middle cerebral artery (MCA) doppler ultrasounds to check the baby’s blood flow. If they see signs of anemia, they can actually perform an intrauterine blood transfusion. They literally give the baby a blood transfusion while it’s still in the womb. It’s mind-blowing science, but obviously, it's better to avoid that stress if you can.
Specific Times You Need to Call the Doctor
It isn't just about the 28-week mark. Life happens. If you are Rh-negative, you need to be hyper-aware of any "mixing" events.
- Vaginal Bleeding: Even a little spotting in the first trimester should be reported.
- Abdominal Trauma: If you trip and fall on your belly or get in a minor car accident, go in. The physical jarring can cause a "fetomaternal hemorrhage."
- External Cephalic Version: If your baby is breech and the doctor tries to manually turn them from the outside, you need a shot.
- Miscarriage or Ectopic Pregnancy: This is the one that breaks my heart. People going through the trauma of a loss often forget the Rh factor. Even if the pregnancy doesn't go to term, you need that shot to protect your future pregnancies.
Managing the Anxiety of an Rh Negative Pregnancy
It’s easy to spiral into "what-ifs." You might wonder if your body is "toxic" to your child. It isn't. Your immune system is just doing its job—it’s just a job you don't want it to do in this specific case.
The testing is simple. Your doctor will run an "antibody screen" at your first prenatal visit. They’re looking to see if you’ve already been sensitized by a previous pregnancy or a mismatched blood transfusion (which is incredibly rare nowadays). If the screen is negative, you’re in the clear for now. You just wait for the 28-week mark.
Interestingly, some new technologies are emerging. In some countries, they use cell-free DNA testing (like the NIPT test used for Down Syndrome) to determine the baby's blood type as early as 10 weeks. If the baby is Rh-negative, the mother can skip the RhoGAM entirely. While this is becoming more common in Europe, many US insurance companies still find it cheaper to just give everyone the shot rather than pay for the expensive genetic blood type test.
Actionable Steps for Your Pregnancy Journey
If you've just seen that "Rh Negative" result on your lab portal, here is exactly what you need to do.
First, confirm the biological father's blood type. If he is 100% Rh-negative, you can breathe a massive sigh of relief and mostly ignore this entire issue. If he is Rh-positive or if his blood type is unknown, you need to be vigilant.
Second, check your medical records for any past "events." Did you have an abortion, a miscarriage, or an ectopic pregnancy where you didn't get a shot? Tell your OB-GYN immediately. They need to know if there's a chance you're already sensitized.
Third, put a reminder in your phone for your 26-week appointment to discuss the RhoGAM schedule. Don't assume the office will remember—offices get busy. Being your own advocate is key.
💡 You might also like: Where did the Black Plague start? The messy truth about the 1340s
Finally, if you experience any bleeding or trauma, don't "wait and see." Call the on-call nurse. Tell them clearly: "I am Rh-negative and I've had a potential exposure event." This ensures you get the treatment within that critical 72-hour window.
This is one of the few things in pregnancy that has a near-perfect "fix." By staying on top of the shots, the risk of your baby developing Rh disease drops to less than 1%. Focus on your prenatal vitamins, your nursery colors, and getting some sleep. Modern medicine has the Rh factor covered.