It starts with a weird, electric zapping in your brain. Some people call them "brain shivers." Others describe them as "brain zaps." Whatever the name, it feels like a tiny lightning bolt just flicked the back of your skull. If you’ve ever tried to taper off duloxetine, you know exactly what I’m talking about. Honestly, the side effects from Cymbalta withdrawal can feel like a full-body mutiny.
People take Cymbalta—the brand name for duloxetine—for all sorts of reasons. Maybe it was for major depressive disorder. Perhaps it was chronic back pain or fibromyalgia. It’s a powerhouse of a drug, an SNRI (serotonin-norepinephrine reuptake inhibitor) that tinkers with the very chemistry of how your nerves talk to each other. But here is the thing: your brain gets used to that help. It gets comfortable. When you try to take that support away, even slightly too fast, the nervous system panics.
It’s not just "in your head," even though that’s where the zaps live. It’s a systemic physiological reaction.
Why Side Effects from Cymbalta Withdrawal are So Intense
You have to understand the half-life. Cymbalta has a notoriously short half-life, usually cited around 12 hours. This means the medication leaves your bloodstream significantly faster than drugs like Prozac, which can linger for weeks. When the concentration drops off a cliff, your receptors are left screaming for the chemical stability they’ve known for months or years.
The FDA-approved labeling acknowledges "Discontinuation Syndrome," but many patients feel that clinical term undersells the reality. It’s not just a "syndrome." For some, it’s a debilitating weeks-long marathon of nausea, vertigo, and what feels like a total personality transplant.
The "Brain Zap" Phenomenon
Researchers still aren't 100% sure why brain zaps happen. The leading theory involves the sudden fluctuation of serotonin levels affecting the way the brain processes sensory input. It’s often triggered by moving your eyes from side to side. You look left to see who walked into the room, and bzzzt—a localized electric shock. It's jarring. It's scary if you don't know it's coming.
👉 See also: What to Do for Kidney Stones at Home: Why Water Isn't Always Enough
The Physical Toll Nobody Mentions
Most medical brochures list "nausea" and "dizziness." That's the PG version. The reality of side effects from Cymbalta withdrawal is often much more visceral. We are talking about "sea sickness" that doesn't stop when you sit down.
- Digestive Chaos: Since a huge portion of your body's serotonin is actually in your gut, withdrawal often leads to intense cramping, diarrhea, or a complete loss of appetite.
- The Cold Sweats: You might wake up at 3:00 AM drenched, shivering, yet feeling like your skin is on fire. It’s a thermoregulation glitch.
- Vertigo: This isn't just feeling lightheaded. It's the sensation that the floor is tilting 45 degrees while you’re trying to brush your teeth.
I’ve heard stories of people having to crawl to the bathroom because the room wouldn’t stop spinning. That is the level of intensity we're dealing with here. It is a physical dependency—not an addiction in the "craving" sense, but a physiological reliance that requires a very slow, very respectful exit strategy.
Emotional Volatility and the "Cymbalta Rage"
This is the part that ruins relationships. You might find yourself screaming at a cereal box because it didn’t open correctly. This "Cymbalta rage" is a documented, though often dismissed, side effect of tapering too quickly.
Your norepinephrine levels are fluctuating wildly. This is the "fight or flight" chemical. When it's out of whack, your fuse becomes non-existent. You aren't "depressed" again; you are experiencing a chemical rebound. You might feel "flat" one hour and then burst into uncontrollable sobbing the next because you saw a stray cat on a commercial. It's exhausting for the patient and confusing for their family.
👉 See also: Why it okay not to be okay is the most honest thing you can tell yourself right now
The Myth of the Two-Week Taper
Many doctors, following standard pharmaceutical guidelines, suggest a two-week taper. For many, this is way too fast. Dropping from 60mg to 30mg is a 50% reduction in one go. To your brain, that’s a massive shock.
Strategies That Actually Work (According to the Community)
There is a massive community of "survivors" online—groups like Cymbalta Withdrawal Survivor Support—where people share what actually helped them when medical advice felt insufficient. One of the most famous, albeit controversial, methods is "bead counting."
Cymbalta capsules are filled with tiny enteric-coated pellets. Because the manufacturer doesn't make 5mg or 1mg doses, some patients literally open the capsules and remove a few beads every day, slowly decreasing the dose by 1% or 2% a week.
Note: You should never do this without talking to a pharmacist or a doctor who understands the complexity of SNRI discontinuation. Opening capsules can affect how the drug is absorbed in the stomach, but for those who cannot tolerate the standard 30mg-to-zero jump, it has been a literal lifesaver.
- Hydration is non-negotiable. Your nervous system is stressed; don't make it fight dehydration too.
- Omega-3 Supplements. Some anecdotal evidence and small-scale studies suggest high-quality fish oil can help dampen the intensity of brain zaps.
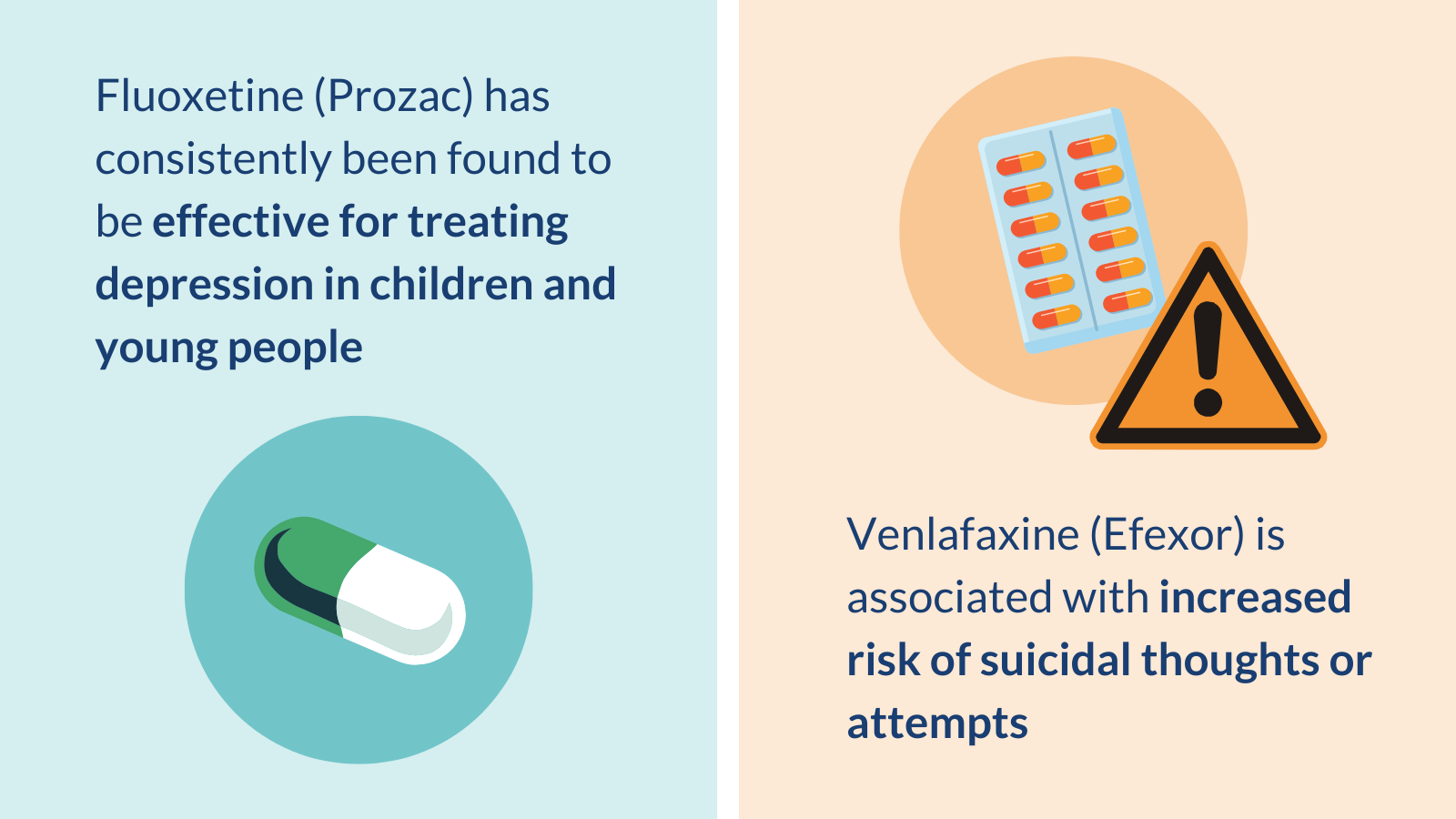
- The "Bridge" Method. Sometimes, a doctor will cross-taper you onto a medication with a longer half-life, like Prozac (fluoxetine), to "cushion" the fall as the Cymbalta leaves your system.
The "Black Box" Reality
Cymbalta carries a FDA black box warning for a reason. While primarily focused on suicidal ideation in young adults, the volatility of withdrawal can also trigger dark thoughts in people who never had them before. If you start feeling like you're in a dark hole with no exit during your taper, that is the drug talking. It is not "you."
It is vital to have a support person. Someone who knows you’re tapering and can tell you, "Hey, you’re just having a withdrawal symptom," when you start spiraling.
Moving Forward Safely
If you are currently staring at a bottle of 60mg capsules and feeling terrified, take a breath. It is possible to get off this medication. The key is patience. Most people get into trouble because they are in a rush to be "clean" of the drug.
Actionable Steps for a Successful Transition:
- Log Everything: Keep a daily symptom journal. Rate your brain zaps and nausea on a scale of 1-10. This helps you see that the "bad days" are actually getting further apart, even when it doesn't feel like it.
- The 10% Rule: Many advocates suggest never dropping your dose by more than 10% of your current dose per month. It takes longer, but it keeps you functional.
- Prioritize Sleep: Withdrawal-induced insomnia is real. Use magnesium or whatever gentle sleep aid works for you, because everything feels ten times worse when you’re sleep-deprived.
- Consult a Compounding Pharmacist: If bead counting sounds like a nightmare, a compounding pharmacy can often create custom, low-dose capsules (e.g., 27mg, 24mg, 21mg) to allow for a smooth, professional taper.
The side effects from Cymbalta withdrawal are a testament to how powerful these neurological tools are. They change us. And when we decide to move on from them, we have to give our brains the time and grace to find their own balance again. You wouldn't jump out of a moving car; you slow it down to a crawl first. Treat your brain with that same level of caution.
Keep your doctor in the loop, even if you have to advocate hard for a slower taper than they initially suggested. Your stability is the only metric that matters.