You’ve seen the movies. A man gasps, clutches his chest with a white-knuckled grip, and falls face-first onto the sidewalk. It’s dramatic. It’s sudden. It’s also, quite frankly, a bit of a lie. While that "Hollywood Heart Attack" definitely happens, real life is usually much more subtle, confusing, and—honestly—easy to ignore until it’s almost too late.
The truth is that signs of a heart attack don't always feel like "pain." People often describe it as a weird pressure, or maybe just a nagging sense that something is "off" in their torso. I've talked to patients who thought they just had bad Burrito-induced heartburn. They took an antacid and went to bed, not realizing their heart muscle was literally starving for oxygen.
We need to stop waiting for the "big one" and start paying attention to the quiet signals. Your body is remarkably good at signaling distress, but it doesn't always use a megaphone. Sometimes it just whispers.
Why We Miss the Early Warning Signals
If you’re looking for a crushing sensation, you might miss the slow burn. The American Heart Association notes that many heart attacks start slowly, with mild pain or discomfort. It isn't always a light switch flipping off; it's often a dimmer switch slowly lowering.
One of the biggest issues is the "denial factor." Humans are hardwired to hope for the best. You tell yourself it’s just a pulled muscle from the gym or maybe you’re just coming down with a flu. This is especially true for women.
✨ Don't miss: I Want to Disappear: Why Your Brain Craves the Exit Button
Research from the Lancet has repeatedly shown that women are less likely to experience the classic chest-clutching symptoms. Instead, they might feel an overwhelming, bone-deep exhaustion. Imagine trying to walk through waist-deep molasses. That kind of tired. Or maybe it’s a sharp pain in the neck or jaw. Because these don't fit the "standard" image of a heart attack, women often wait longer to seek help, which leads to worse outcomes. It’s a systemic misunderstanding of biology that costs lives every single year.
The Weird Places You Feel Signs of a Heart Attack
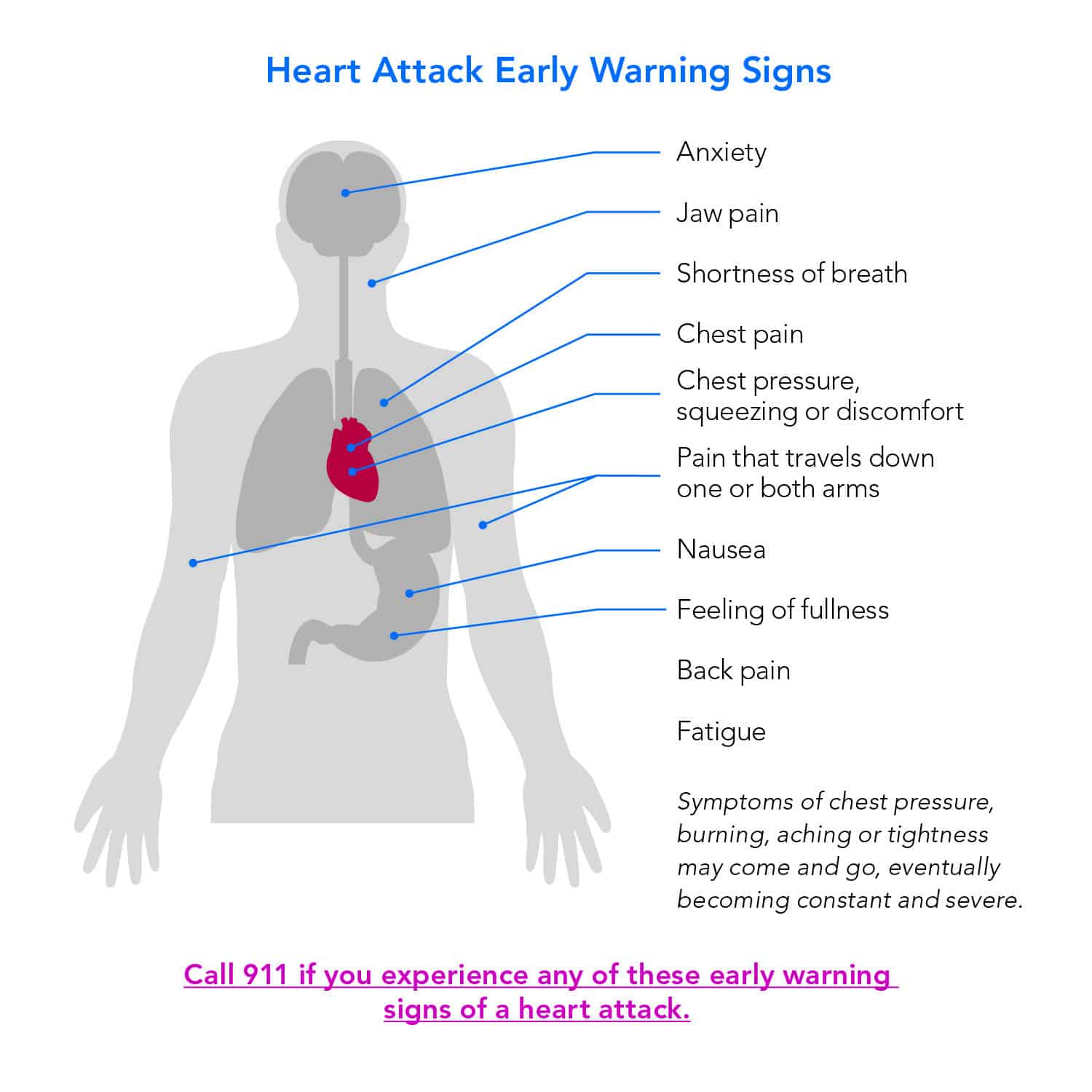
Your nervous system is a bit of a messy switchboard. When the heart is in trouble, the nerves sending those distress signals share the same pathways as nerves from your arms, jaw, and back. This is called "referred pain."
Basically, your brain gets the signals crossed.
- The Left Arm (And Sometimes the Right): Most people know about the left arm. But did you know it can be both? Or just the right? It’s often a dull ache that radiates down toward the wrist.
- The "Toothache" That Isn't: I've heard stories of people calling their dentist because of a throbbing jaw. If that jaw pain comes on suddenly during physical exertion and vanishes when you sit down, that’s not a cavity. That’s your heart.
- The Upper Back: This feels like a literal knife between the shoulder blades. It’s common in women and often dismissed as "carrying stress" or poor posture at a desk.
- The Stomach Trap: Nausea and indigestion are huge red flags. If you are breaking out in a cold sweat while feeling like you need to throw up, and you haven't eaten anything suspicious, stop what you’re doing.
It’s not just about where the pain is, though. It’s about the "plus-ones." A heart attack rarely travels alone. If you have chest pressure plus shortness of breath, or jaw pain plus a cold sweat, the math starts looking very grim.
Understanding the "Soft" Symptoms
We need to talk about "prodromal" symptoms. These are the signs that show up days or even weeks before the actual event. Think of them as the tectonic plates shifting before the earthquake hits.
👉 See also: Dog Tick Prevention: What Most Owners Get Wrong About Meds
A study published in Circulation found that many women reported unusual fatigue, sleep disturbances, and shortness of breath up to a month before their heart attack. This isn't the "I stayed up too late watching Netflix" tired. This is the "I can't make it from the couch to the fridge without catching my breath" tired.
The lightheadedness is another big one. If the room starts spinning or you feel faint for no apparent reason, your heart might be struggling to pump enough blood to your brain. This often happens because of an arrhythmia or a sudden drop in blood pressure caused by the failing muscle. It’s your body’s way of saying, "Hey, we’re losing pressure in the system here."
What’s Actually Happening Inside?
To understand the signs of a heart attack, you have to visualize the plumbing. Most heart attacks occur due to Coronary Artery Disease. Over decades, gunk—clinically known as plaque—builds up on the inner walls of your arteries. This plaque is made of cholesterol, fats, and calcium.
Usually, the trouble starts when a piece of that plaque ruptures.
Think of it like a blister popping inside your artery. Your body sees that rupture as an injury and rushes to form a blood clot to "heal" it. But in a narrow artery, that clot acts like a cork in a bottle. It completely blocks the blood flow.
Downstream from that blockage, the heart muscle begins to die. It doesn't take long. After about 20 minutes of total blockage, the damage starts becoming irreversible. This is why cardiologists say "Time is Muscle." Every minute you spend debating whether or not to call 911 is a minute where more of your heart tissue is potentially turning into non-functional scar tissue.
📖 Related: How Can I Shadow a PA Without Getting Ignored or Rejected?
Risk Factors vs. Reality
We all know the usual suspects: smoking, high blood pressure, and high LDL cholesterol. These are the "big three." But life is rarely that simple.
You can be a marathon runner and still have a heart attack. Genetic factors like Lipoprotein(a)—often called "Lp-little-a"—can make your blood more likely to clot or your arteries more likely to build up plaque, regardless of how much kale you eat. Stress is another silent killer. Chronic stress keeps your cortisol levels high and your blood vessels constricted. If you’re living in a constant state of "fight or flight," your heart is essentially running a marathon while you’re just sitting at your desk.
Also, let’s talk about diabetes. If you have diabetes, your nerves might be damaged (neuropathy). This can actually mask the pain of a heart attack. You might have what’s called a "silent" heart attack where you feel almost nothing at all, or perhaps just a slight sense of weakness. It’s terrifying because the damage is just as real, but the warning system is broken.
Immediate Action: What to Do Right Now
If you suspect you or someone else is experiencing signs of a heart attack, the clock is your enemy.
- Call 911 Immediately: Do not drive yourself to the hospital. If you black out behind the wheel, you're a danger to everyone. Paramedics can start treatment—like performing an EKG and administering medications—the moment they arrive.
- Chew an Aspirin: Unless you are allergic or have been told by a doctor never to take it, chew a full-strength (325mg) aspirin. Chewing it gets it into your bloodstream faster than swallowing it whole. It helps thin the blood and can potentially break up or slow the growth of the clot.
- Sit Down and Stay Calm: Stop all physical activity. Your goal is to decrease the workload on your heart. Loosen tight clothing and try to breathe deeply.
Don't worry about being "wrong." Emergency room doctors would much rather tell you that you have bad gas than have you arrive too late to save your heart muscle. There is no shame in a false alarm when the stakes are literally life and death.
Actionable Steps for Future Prevention
Knowing the signs is the second line of defense. The first is making sure those signs never have a reason to appear.
Get a full blood panel that includes more than just basic cholesterol. Ask your doctor for a hs-CRP (High-Sensitivity C-Reactive Protein) test to check for inflammation in your arteries. Consider a Calcium Scoring CT scan if you are over 40; it’s a quick, non-invasive way to see if there is actual hard plaque building up in your heart’s vessels before it causes a problem.
Monitor your blood pressure at home. The "white coat effect" often makes blood pressure spike at the doctor's office, giving an inaccurate reading. Keeping a log of your resting pressure during a quiet evening on the couch gives a much truer picture of your cardiovascular health.
Finally, listen to your "gut." Many survivors say they just had a "sense of impending doom." It sounds unscientific, but your subconscious picks up on internal physiological shifts before your conscious mind can put a name to them. If you feel like something is fundamentally wrong with your body, act on it. Your heart will thank you.