When you think about the epicenter of the HIV epidemic, your mind probably goes to the 1980s or maybe a major global hub like Sub-Saharan Africa. But honestly, the reality of the highest HIV rate in US jurisdictions today is much closer to home—and it’s probably not where you’d expect.
We often assume that massive, liberal cities like New York or San Francisco are still the front lines. They aren't. While those cities have high numbers of people living with the virus, the actual rate of new infections has shifted dramatically. If you're looking at where the fire is burning hottest in 2026, you have to look at the American South.
The Numbers That Actually Matter
Let’s get the big one out of the way. Washington, D.C. consistently clocks in with the highest HIV rate in the US when looking at new diagnoses per 100,000 people. Recent CDC data and local reports show D.C. sitting at a rate of roughly 32.6 per 100,000. That’s nearly three times the national average.
But D.C. is an outlier because it's a single city-district. When we talk about states, Georgia usually takes the crown with a rate around 25.5. Florida, Louisiana, and Mississippi are right behind it. Basically, if you draw a line across the bottom third of the country, you're looking at the most impacted region in the Western world.
Why the South?
You’ve probably heard people blame "lifestyle choices," but that’s a lazy answer. The real reason the South is struggling is a messy mix of policy, poverty, and a lack of Medicaid expansion.
States like Georgia and Mississippi have some of the highest poverty rates in the country. If you can't afford a car, how are you getting to a clinic that’s 40 miles away? If your state didn't expand Medicaid, how are you paying for PrEP (Pre-Exposure Prophylaxis) or the labs needed to stay on it?
Then there's the stigma. In many Southern communities, HIV is still treated like a moral failing rather than a manageable chronic condition. This keeps people from getting tested. You can't treat what you don't know you have. In 2024, the South had the lowest "PrEP-to-need" ratio in the nation—only about 12 users for every one new diagnosis. Compare that to the Northeast, where the ratio is much higher, and you see the gap clearly.
The Cities Hitting the Red Zone
If we zoom in on metro areas, the list is even more specific. Miami, Florida and Memphis, Tennessee are consistently at the top. Atlanta is right there too. In the Atlanta metro area, the rate of new diagnoses is roughly 25.4 per 100,000.
"That rate is two times greater than all other metropolitan areas and two and a half times higher than the rate nationwide." — Jeff Cheek, Director of the Fulton County Department of HIV Elimination.
It’s wild. Parts of downtown Atlanta have prevalence rates that look more like developing nations than a US tech hub. In Fulton County, nearly 1 in 50 people is living with HIV. That’s a staggering density.
Who Is Actually Getting Hit?
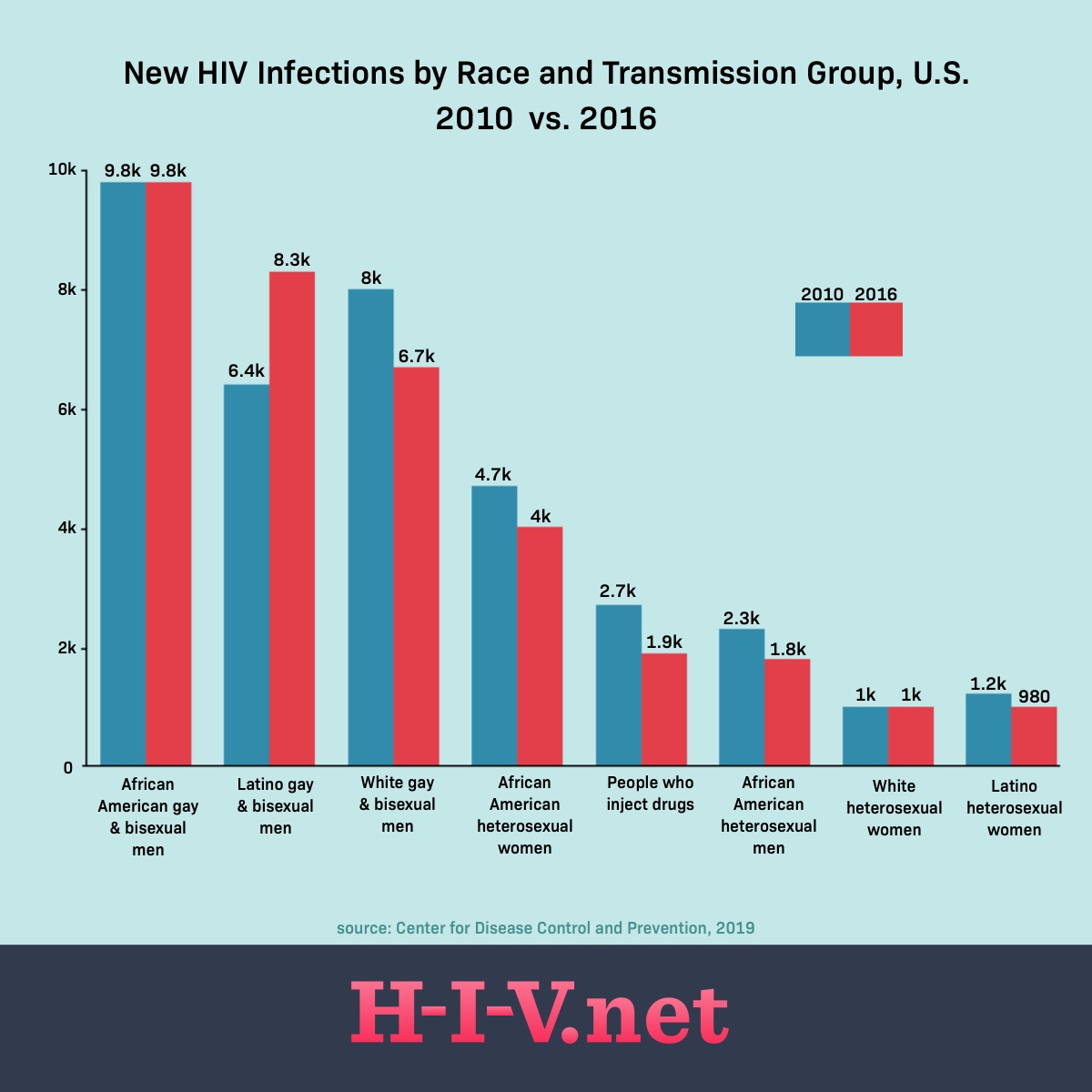
The data is pretty brutal when it comes to racial disparities. Black Americans make up about 12% of the US population but account for nearly 38% of new HIV diagnoses.
Among Black men who have sex with men (MSM), the lifetime risk of contracting HIV has been estimated as high as 50% in certain studies. This isn't because of "riskier behavior"—studies show Black MSM often have fewer partners than their White counterparts. It's about the "network effect." If the virus is more prevalent in your community and you have less access to healthcare, the statistical chance of exposure goes through the roof every time you have a new partner.
The "Ending the HIV Epidemic" (EHE) Reality Check
The government had this big goal: reduce new infections by 75% by 2025 and 90% by 2030.
We aren't there.
While new infections dropped about 12% between 2018 and 2022, progress has been uneven. In 2026, we're seeing some scary headwinds. There are proposed cuts to federal HIV funding, and some states are making it even harder to get on Medicaid. If we pull the rug out from under these programs now, those rates in Georgia and Florida are going to spike again.
What’s Working (And What’s Not)
The good news? We have the tools. U=U (Undetectable = Untransmittable) is a scientific fact. If someone stays on their meds and their viral load is undetectable, they cannot pass the virus to a partner through sex. Period.
🔗 Read more: The Real Story Behind Like Some Who Take Testosterone NYT: Beyond the Hype
The bad news? Access is the bottleneck.
- Long-acting injectables: These are amazing. Instead of a daily pill, you get a shot every couple of months. It’s a game-changer for people with unstable housing or who just hate the daily reminder of the virus.
- Tele-PrEP: Being able to get your HIV prevention meds via a video call has helped rural areas, but you still need labs done.
- Self-Testing: Mail-order tests have helped, but they don't always lead to "linkage to care"—which is the fancy way of saying "getting someone into a doctor's office."
Misconceptions to Throw Away
One thing that drives me crazy is the idea that HIV is a "young person's problem." Actually, new infections among people aged 13-24 have dropped by about 30%. That’s a huge win!
The group where it’s actually rising? People in their 30s and 40s. Also, White women and teenage girls saw a 21% increase in new infections recently. This virus doesn't care about the stereotypes we've built up over the last 40 years. It goes wherever the gaps in healthcare are.
How to Navigate the Risk
If you live in a high-rate area like Atlanta, Miami, or D.C., you sort of have to be your own advocate. Don't wait for a doctor to offer a test. Most doctors still don't bring it up unless you "look" like you're at risk.
- Get a baseline test. It should be part of your yearly physical, but it usually isn't unless you ask.
- Look into PrEP. If you're sexually active and not in a monogamous relationship with someone who is definitely negative, PrEP is a literal lifesaver. It reduces sexual transmission risk by about 99%.
- Use AIDSVu. It's a website that lets you see the HIV rates down to the ZIP code level. It’s eye-opening and helps you understand the local landscape.
- Support Medicaid expansion. If you live in a state that hasn't expanded it, your neighbors are literally dying because of it.
The highest HIV rate in US zones isn't a permanent mark of shame. It's a map of where we've failed to provide basic healthcare. Whether we actually end this epidemic by 2030 depends entirely on whether we decide to fund the solutions we already have.
Next Steps for Your Health:
Check your local health department's website for "Fast Track City" initiatives, which often provide free or low-cost PrEP and testing regardless of your insurance status. If you are in a high-incidence area like the Deep South, look for community-based organizations (CBOs) like the Southern AIDS Coalition; they often have more resources and less red tape than traditional state clinics.