You might think you know what tuberculosis looks like. Most people picture a Victorian-era poet coughing into a lace handkerchief or a dramatic scene from a period movie. It’s scary. It’s visible. But here is the thing: for about a quarter of the entire human population, tuberculosis is a silent passenger. It's just sitting there. No coughing, no fever, no lace handkerchiefs.
This brings us to the massive, often misunderstood gap in tuberculosis infection vs disease.
If you’ve recently tested positive on a skin test or a blood draw, you’re probably spiraling. You’re wondering if you’re contagious or if your lungs are currently being destroyed. Take a breath. Most of the time, a positive test doesn't mean you're "sick" in the way we usually mean it. It means you have a latent infection. There is a world of difference between carrying the bacteria and actually having the disease, and honestly, confusing the two is exactly how stigma spreads.
The Sleeping Giant: What Latent TB Really Is
Think of Latent TB Infection (LTBI) as a standoff.
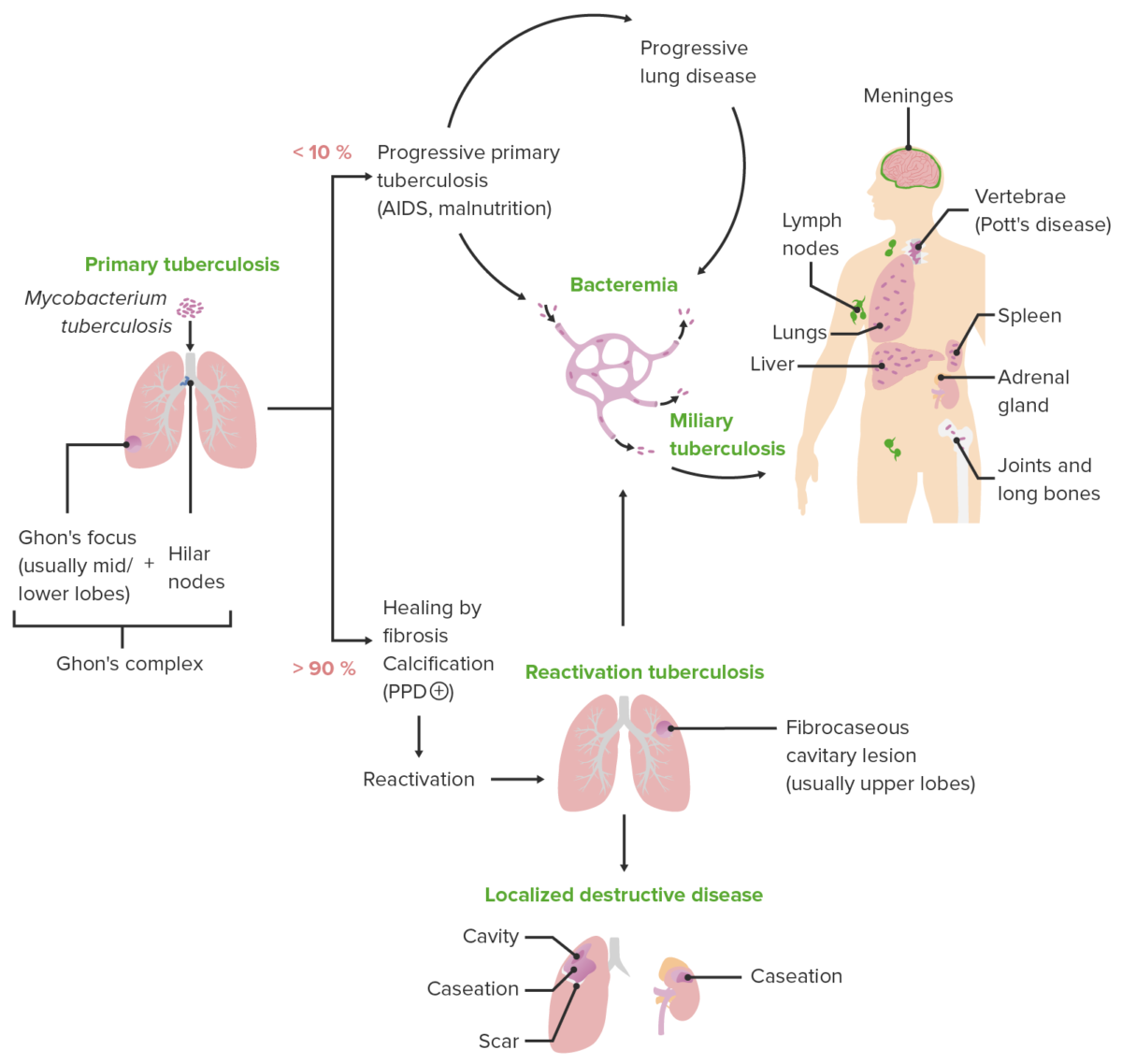
Inside your body, the Mycobacterium tuberculosis bacteria have entered the lungs. Your immune system, which is incredibly efficient when it’s healthy, basically says "not today." Special immune cells called macrophages surround the invaders and wall them off like a biological prison. The bacteria are alive, but they are inactive. They aren't multiplying. They aren't eating your tissue.
You feel fine. Seriously. You could run a marathon, go to work, and kiss your kids without any risk to them. Because the bacteria are locked away, you aren't contagious. You can't spread it.
The CDC notes that people with latent TB have no symptoms. Your chest X-ray will almost always look completely normal. The only way you’d ever know the bacteria are there is through a TST (tuberculin skin test) or an IGRA (interferon-gamma release assay) blood test. These tests don't look for the bacteria itself; they look for your immune system's "memory" of the bacteria.
Why doctors still worry about a "silent" infection
You might wonder why, if you aren't sick and can't spread it, doctors still want to put you on a four-to-nine-month regimen of antibiotics like Rifampin or Isoniazid.
It’s about the future.
About 5% to 10% of people with latent tuberculosis will eventually develop the active disease if they don't get treated. It’s a ticking clock. If your immune system weakens due to age, diabetes, HIV, or even certain medications like biologics for rheumatoid arthritis, the "prison walls" can crumble. The bacteria wake up.
When the Bacteria Wake Up: Active TB Disease
This is the version of tuberculosis everyone fears. When the immune system can no longer contain the bacteria, they begin to multiply rapidly. They start breaking down the tissue in the lungs—or sometimes the kidneys, spine, or brain.
When we talk about tuberculosis infection vs disease, the "disease" part is the clinical illness. You are sick. You are also, most likely, infectious.
The symptoms aren't subtle, though they can mimic a bad flu or pneumonia at first:
- A cough that lasts three weeks or longer.
- Chest pain.
- Coughing up blood or sputum (phlegm from deep inside the lungs).
- Weakness or fatigue.
- Unexplained weight loss (this is why they used to call it "Consumption").
- Chills and fever.
- Drenching night sweats.
If you have these symptoms and a positive test, the bacteria are no longer latent. They are active. At this point, you become a public health priority. You'll likely be isolated for a few weeks until the medication reduces your bacterial load enough that you aren't a risk to others.
🔗 Read more: Blue Waffle STD Real Image: Why This Viral Hoax Still Tricks People
The Science of the Shift: Why Does it Progress?
It isn't random.
The shift from tuberculosis infection vs disease usually happens when the body's defenses are compromised. According to the World Health Organization (WHO), people living with HIV are 16 times more likely to fall ill with active TB. But it isn't just HIV.
Diabetes is a huge, under-discussed factor. High blood sugar actually impairs the way your white blood cells move and hunt bacteria. Tobacco use also skyrockets the risk. Smoking damages the cilia in your lungs—the tiny hairs that sweep out debris—making it much easier for a latent infection to turn into a full-blown disaster.
Then there’s the timing. The risk of progression is highest in the first two years after the initial infection. If you were recently exposed to someone with active TB and you test positive, your doctor is going to be much more aggressive about treatment than if you had a positive test twenty years ago and have stayed healthy ever since.
Testing Nuances: How We Tell the Difference
This is where things get kind of technical, but stay with me.
If you go to a clinic and your skin test comes back with a hard, raised bump (induration), the nurse will measure it in millimeters. They don't just care if it's "positive"; they care how positive it is based on your risk factors.
Once you have that positive test, the very next step—always—is a chest X-ray or a sputum sample.
This is the "fork in the road" for tuberculosis infection vs disease.
- Positive Test + Normal X-ray + No Symptoms = Latent TB Infection.
- Positive Test + Abnormal X-ray + Coughing/Fever = Active TB Disease.
It’s a simple diagnostic path, but it’s vital. You cannot treat active TB with a single-drug latent TB protocol. If you do that, you risk creating drug-resistant TB, which is a global health nightmare. Active TB requires a "cocktail" of four different drugs (usually Isoniazid, Rifampin, Ethambutol, and Pyrazinamide) taken for at least six months.
The "BCG Vaccine" Complication
If you grew up outside the United States, you might have received the BCG vaccine.
This vaccine is great for protecting kids against severe forms of TB, but it messes with the skin test. It can cause a "false positive." This is why many modern clinics prefer the IGRA blood test (like QuantiFERON-TB Gold). The blood test is much more specific. It doesn't get confused by the vaccine. If your blood test is positive, you have the bacteria in your body. Period.
Treatment is Not Optional (But it’s Easier Than it Used to Be)
Years ago, latent TB treatment was a slog. You had to take Isoniazid every single day for nine months. Most people quit halfway through because, well, they didn't feel sick.
Today, we have "short-course" regimens. There’s a protocol called 3HP—a combination of Isoniazid and Rifapentine taken once a week for just 12 weeks. It’s a game-changer. It’s much easier on the liver and much easier to finish.
If you have active disease, the stakes are higher. You might be put on "Directly Observed Therapy" (DOT). This sounds intense because it is: a healthcare worker literally watches you swallow your pills. It isn't because they don't trust you; it’s because missing doses of active TB meds is how we get Multi-Drug Resistant TB (MDR-TB). If the bacteria learn how to fight the drugs, we lose our best weapons.
Real-World Impact: More Than Just a Lab Result
We need to talk about the "lifestyle" side of this.
If you are diagnosed with latent TB, your life doesn't really change. You go to work. You go to the gym. You just take a pill.
But if you are diagnosed with active TB, your world stops for a bit. The health department gets involved. They will ask for a list of everyone you’ve spent time with. They will test your family, your coworkers, and your friends. It can feel invasive and embarrassing.
The tragedy is that many people hide their symptoms because they are afraid of this process. They wait until they are severely ill to seek help. By then, they’ve often passed the infection to the people they love most.
Understanding the distinction between tuberculosis infection vs disease helps break this cycle. If we normalize testing and treating the latent version, we prevent the active version from ever happening.
Actionable Steps for the Newly Diagnosed
If you just found out you have a positive TB test, don't panic. Follow these steps to navigate the system:
1. Confirm the Diagnosis
If you had a skin test and you’ve had the BCG vaccine, ask for a QuantiFERON or T-Spot blood test. It’s more accurate and avoids false positives.
2. Get the Imaging
Ensure you get a high-quality chest X-ray. If you have any symptoms at all—even a mild persistent cough—make sure the doctor knows. They might want to test your sputum (the stuff you cough up) to see if bacteria are actually present.
3. Evaluate Your Risks
Be honest with your doctor about your health history. Do you have diabetes? Do you drink alcohol heavily? (Alcohol can increase liver toxicity during treatment). Are you on any immune-suppressing meds? This determines which treatment plan is safest for you.
4. Commit to the Regimen
Whether it’s the 12-week or 9-month plan, do not stop halfway. If you stop early, the strongest bacteria survive and can come back much harder to kill later.
5. Protect Your Circle
If you are diagnosed with the active disease, follow the isolation protocols strictly. Usually, after two weeks of consistent medication, you are no longer contagious, but you need a doctor to clear you first.
👉 See also: Spironolactone Before and After Facial Hair: What Most People Get Wrong About Hirsutism
Tuberculosis is an ancient disease, but it isn't a death sentence. It’s a manageable condition, provided you know which side of the line you’re on. Latent infection is a warning; active disease is a crisis. Both are treatable.
The biggest mistake is doing nothing. If you carry the bacteria, treat it while it's sleeping. Don't wait for it to wake up.
Sources and Further Reading
- Centers for Disease Control and Prevention (CDC). "Latent TB Infection vs. TB Disease."
- World Health Organization (WHO). "Tuberculosis Profile."
- American Thoracic Society. "Treatment of Latent Tuberculosis Infection in Adults."
- National Institute of Allergy and Infectious Diseases (NIAID). "Tuberculosis (TB) Symptoms and Diagnosis."