The sky turns a bruised shade of grey around 4:00 PM, and suddenly, getting off the couch feels like wading through wet cement. You're not just "tired." You’re fundamentally heavy. This is the reality of Seasonal Affective Disorder (SAD), a specific type of clinical depression that tracks with the tilt of the earth and the loss of sunlight. For years, the go-to advice has been "get a sun lamp" or "try vitamin D for seasonal depression." But honestly, the relationship between that little gel capsule and your brain chemistry is way more complicated than just popping a pill to replace the sun.
It’s about biology, not just supplements.
Most people treat vitamin D like a standard vitamin, but it’s actually a pro-hormone. Your skin manufactures it when hit by UVB rays, triggering a cascade of chemical reactions that eventually land in your brain's receptors. When the days get short, that factory shuts down.
The Science of the "SAD" Brain and Vitamin D
Why does this matter for your mood? Research published in The Journal of Alimentary Pharmacology and Therapeutics and studies from the University of Toronto have pointed to a pretty clear link: vitamin D receptors are scattered all over the areas of the brain involved in depression, specifically the hippocampus and the anterior cingulate cortex. These are the regions that handle how you process emotions and memories.
👉 See also: Which Sugar Substitute Is The Healthiest? What Most People Get Wrong
When you’re low on the "sunshine vitamin," your brain struggles to regulate serotonin. That’s the "feel-good" neurotransmitter everyone talks about. Low D levels are often found in people struggling with SAD, but here is the kicker: scientists still argue over whether the low vitamin D causes the depression or if the lifestyle of a depressed person—staying indoors, eating poorly—causes the low vitamin D. It’s a bit of a chicken-and-egg situation that hasn't been fully teased apart yet.
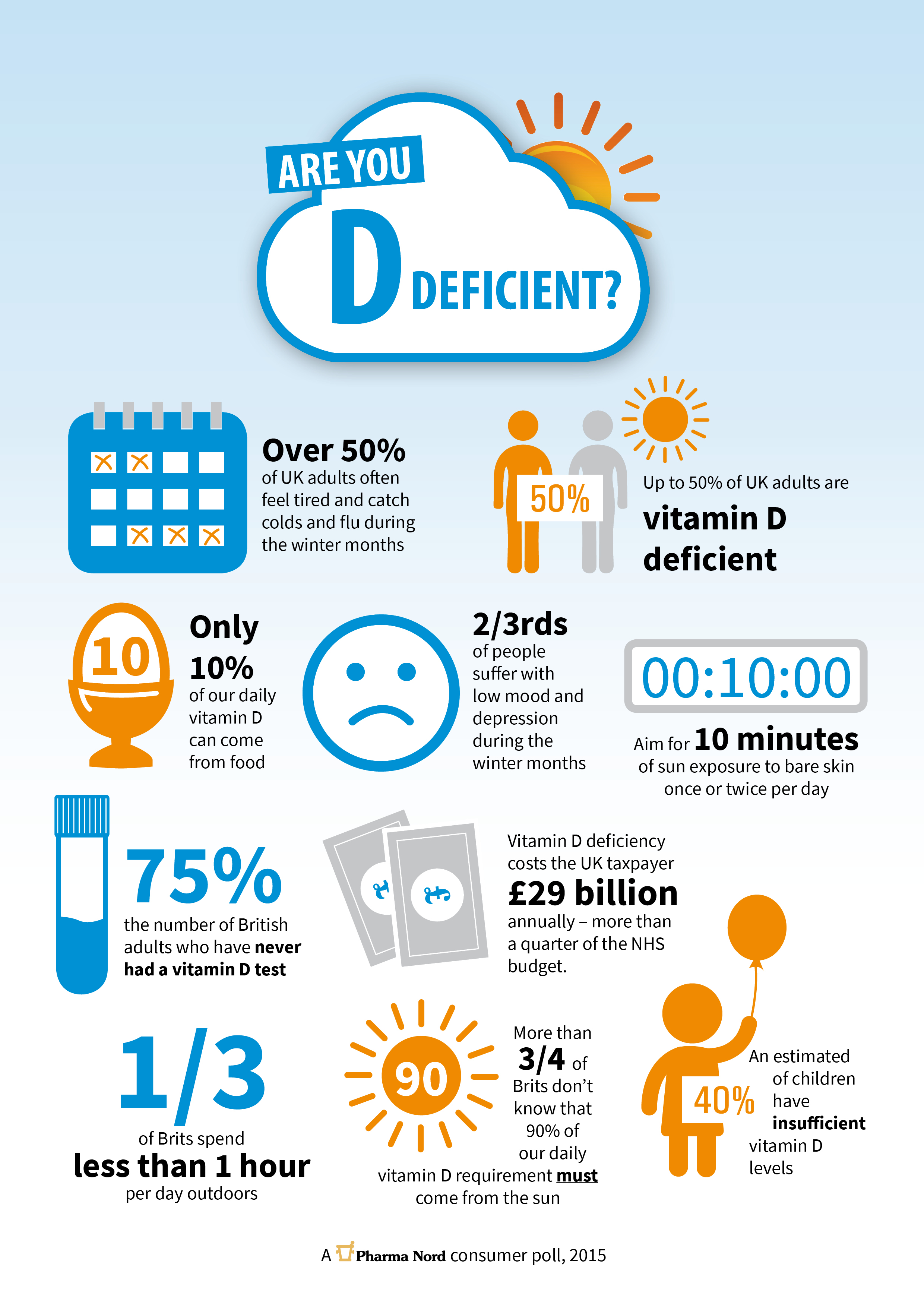
Dr. Michael Holick, a leading expert from Boston University, has spent decades arguing that most of the Northern Hemisphere is essentially living in a state of chronic deficiency from October to March. In places like Seattle, Chicago, or London, the sun is literally at the wrong angle to produce vitamin D in human skin during winter. You could stand outside naked in the snow for three hours and your body still wouldn't make a lick of it.
What the studies actually say
The VITAL study, one of the largest clinical trials of its kind, looked at whether vitamin D3 supplements prevented depression in over 18,000 adults. The results were... underwhelming. They found no significant difference in mood scores for the general population.
Wait. Don't throw your bottle away yet.
🔗 Read more: Calories in a Sargento Cheese Stick: What Your Nutrition Label Isn't Telling You
That study looked at prevention in people who weren't necessarily deficient. When you look at people who are already diagnosed with SAD or clinical depression and have documented low blood levels, the needle moves. A 2014 meta-analysis found that taking vitamin D for seasonal depression showed a benefit comparable to some anti-depressants, but only for those who were truly deficient (levels below 20 ng/mL) at the start.
How much do you actually need?
This is where it gets messy. The RDA (Recommended Dietary Allowance) is 600 to 800 IU per day. Many functional medicine experts, like those at the Vitamin D Council, argue this is laughably low, barely enough to keep your bones from softening, let alone enough to support neurotransmitter function in the brain.
But you can overdo it. Vitamin D is fat-soluble. Unlike Vitamin C, which you just pee out if you take too much, D stores itself in your fat cells. If you take 10,000 IU every day for months without a doctor's supervision, you risk hypercalcemia—basically, too much calcium in your blood, which can wreck your kidneys and heart.
- Get a 25-hydroxy vitamin D test. This is the only way to know where you stand.
- Aim for a "sweet spot." Many experts suggest a range of 40-60 ng/mL for optimal mental health, rather than just the "sufficient" 30 ng/mL.
- Take it with fat. Since it's fat-soluble, taking it with a spoonful of peanut butter or a piece of avocado can increase absorption by up to 50%.
It’s not a magic bullet
Kinda frustrating, right? We want a simple fix. But vitamin D for seasonal depression works best as part of a stack. If you're relying solely on a pill while sitting in a dark room with the curtains closed, you're fighting an uphill battle. Light therapy—using a 10,000 lux lamp—has a much faster effect on the circadian rhythm than supplements do. The supplement is the slow-burn foundation; the light box is the immediate spark.
The Magnesium Connection Nobody Talks About
You can swallow all the D3 in the world, but if you’re low on magnesium, your body can’t convert it into its active form. It just sits there, useless. Most Americans are magnesium deficient because our soil is depleted. If you’re trying to fix your winter blues, you should probably be looking at your magnesium intake too. Think pumpkin seeds, spinach, or a high-quality magnesium glycinate supplement before bed. It helps with the anxiety that often hitches a ride with seasonal depression.
Real World Nuance: Melatonin and the Winter Slump
Seasonal depression isn't just about sadness. It’s about a "phase shift." Your body starts producing melatonin—the sleep hormone—way too early because it gets dark at 4:30 PM. This leaves you feeling like a zombie by dinner time.
💡 You might also like: Sea Salt vs Table Salt: What Most People Get Wrong About Your Shaker
Vitamin D helps regulate the circadian clock, but it’s just one piece of the puzzle. You've also got to look at your "sleep hygiene." Are you staring at a blue-light screen until midnight? That’s doubling down on the biological confusion your brain is already experiencing.
Actionable Next Steps for Hacking the Winter Blues
Stop guessing. If you feel like your mood is tanking every time the leaves fall, do these three things immediately:
- Order a blood panel. Specifically ask for the 25(OH)D test. Don't start "mega-dosing" based on a TikTok video. See where you are starting from.
- Check your Vitamin D3/K2 balance. Taking D3 alone can sometimes lead to calcium depositing in your arteries rather than your bones. Vitamin K2 acts like a traffic cop, moving the calcium to where it belongs. Look for a combined supplement.
- Micro-dose the sun (when it’s there). On the rare days the sun peaks out in February, get outside for 10 minutes without sunglasses. Let that light hit your retinas. It signals your brain to stop producing melatonin and start producing serotonin.
- Pair your D with "Forest Bathing." Or just a walk in the park. Research shows that physical movement in nature, even in the cold, significantly amplifies the effects of vitamin D supplementation on mood.
The bottom line is that vitamin D for seasonal depression is a powerful tool, but it's not a cure-all. It's a physiological necessity that most of us are missing. Fix the deficiency, but don't forget to turn on the lights, move your body, and talk to a professional if the darkness feels too heavy to lift on your own.