You've seen the memes. Someone straightens a pencil on a desk or organizes their spice rack by color and laughs, "I'm so OCD." It is a shorthand for being tidy. Honestly, that's not even close. When we ask what does OCD mean, we aren't talking about a quirk or a personality trait. We are talking about a debilitating mental health condition called Obsessive-Compulsive Disorder. It’s heavy. It’s exhausting. And for the millions of people living with it, it has nothing to do with "liking things clean."
OCD is an anxiety-driven cycle. Imagine your brain gets stuck on a specific, terrifying thought—like a broken record that won't stop skipping. That’s the obsession. To stop the record from skipping, you feel like you must do something specific, like washing your hands or checking the stove ten times. That’s the compulsion. It’s a loop. You’re trapped in it.
The "O" in OCD: Intrusive Thoughts That Won't Leave
Obsessions are the engine of this disorder. They aren't just "worries." Everyone worries about whether they locked the door. A person with OCD doesn't just worry; they experience a visceral, intrusive image of a burglar entering their home and hurting their family because of that unlocked door.
These thoughts are often "egodystonic." That’s a fancy clinical term which basically means the thoughts are the opposite of what the person actually believes or wants. A deeply religious person might have intrusive, blasphemous thoughts. A loving parent might have a flash of an image of harming their child. It’s horrifying for them. These aren't "repressed desires." They are the brain’s alarm system malfunctioning and firing off "danger" signals for no reason.
Common obsessions include:
- Fear of contamination (germs, chemicals, or even "bad luck").
- Perfectionism or a need for things to be "just right" or symmetrical.
- Unwanted sexual or violent thoughts that cause immense guilt.
- Fear of losing control or acting on an impulse.
- Responsibility for harm (the feeling that if you don't do X, someone will die).
The "C" in OCD: Why People Do Things Over and Over
If the obsession is the itch, the compulsion is the scratch. But here’s the kicker: scratching makes the itch worse in the long run. Compulsions are repetitive behaviors or mental acts that a person feels driven to perform in response to an obsession.
The goal? To reduce the anxiety or prevent a dreaded event.
Sometimes the compulsion is logically connected to the fear. If you're afraid of germs, you wash your hands. Simple, right? But often, the compulsion is totally unrelated. Someone might feel they have to tap the table four times to prevent their mom from getting into a car accident. They know, intellectually, that tapping a table doesn't control the universe. But the "what if" is so loud they can't ignore it.
It is Not Always Physical
You can't always see OCD. A lot of it happens behind the eyes. This is sometimes called "Pure O" (though that's a bit of a misnomer because compulsions are still happening; they're just mental). Mental rituals include:
- Mentally reviewing a conversation to ensure you didn't say something offensive.
- Counting to a certain number over and over.
- Praying in a specific way to "undo" a bad thought.
- Seeking reassurance from others ("Are you sure I'm a good person?").
Why the "Neat Freak" Stereotype is Actually Harmful
When we reduce what does OCD mean to "liking things organized," we erase the suffering of people whose lives are falling apart because of the disorder.
I once talked to a man who spent four hours every morning checking his car tires for "blood" because he was convinced he had accidentally hit someone on his way home. He wasn't a "neat freak." He was a man in agony. He lost his job because he couldn't get to work on time.
The stereotype also prevents people from getting diagnosed. If your OCD manifests as "scary thoughts about harming people," you aren't going to think you have OCD if the only thing you know about it is that people with OCD like clean desks. You're just going to think you're a monster. You’ll stay silent. You’ll suffer longer.
What Causes the Brain to Get Stuck?
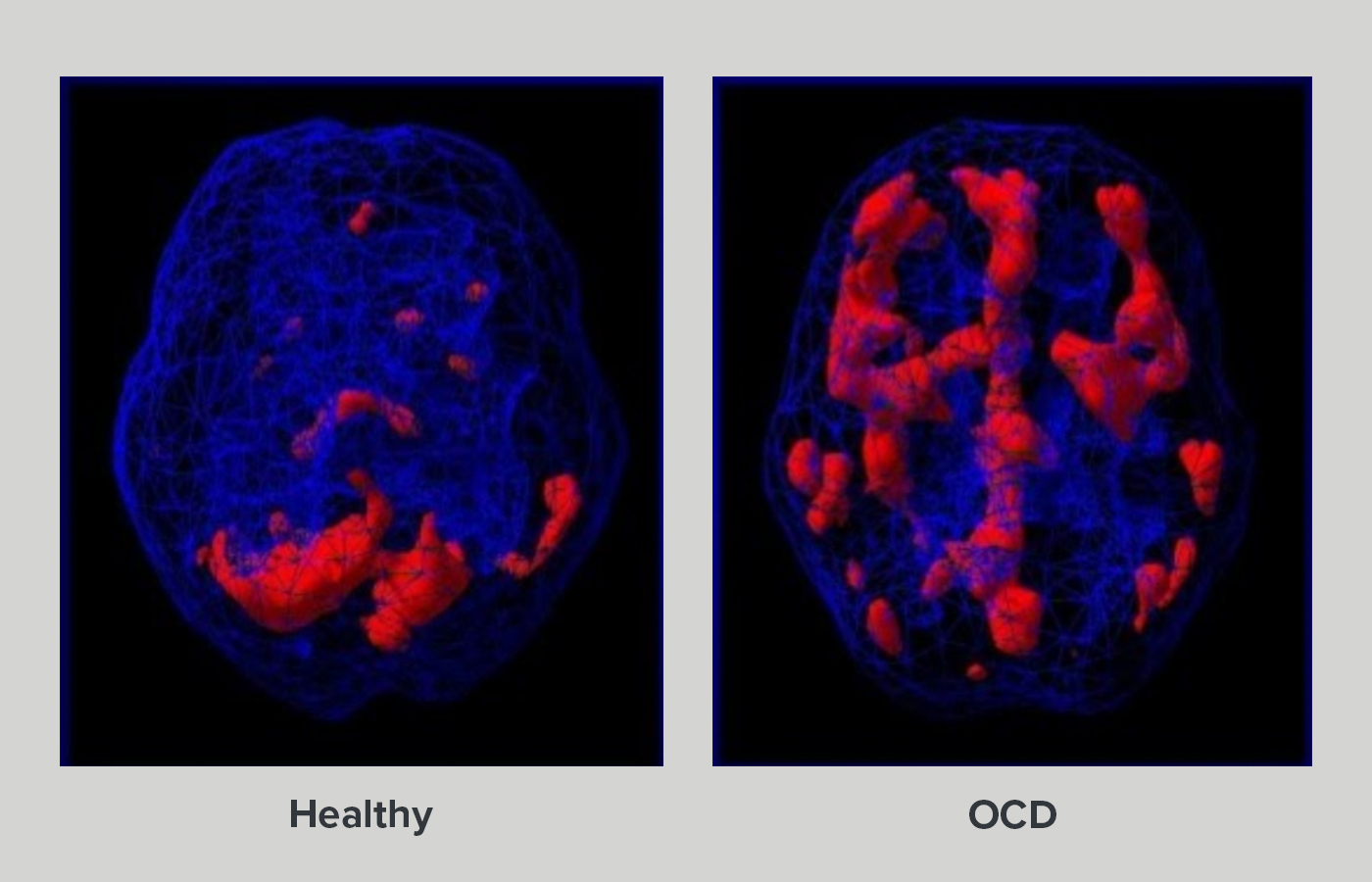
We don't have a single "smoking gun" for why OCD happens. It is likely a cocktail of genetics, brain chemistry, and environment. Research points toward communication issues between the front part of the brain (the orbitofrontal cortex) and deeper structures (the basal ganglia). These areas use serotonin to talk to each other. When that communication breaks down, the brain's "error detection" system stays on "High Alert" even when there's no error.
🔗 Read more: What Is Good for Leg Cramps at Night: Dealing With the 2 AM Charlie Horse
Studies from the National Institute of Mental Health (NIMH) suggest that if a parent or sibling has OCD, your chances of developing it are higher. It’s not a choice. It’s not a lack of willpower. It is a physiological glitch.
Real Treatment: ERP is the Gold Standard
You can't just "stop thinking about it." If someone tells you that, they don't get it.
The most effective treatment is something called Exposure and Response Prevention (ERP). It’s a type of Cognitive Behavioral Therapy (CBT). It sounds scary because it is. You basically work with a therapist to face your fear (the exposure) and then—this is the hard part—you don't do the ritual (the response prevention).
If you're afraid of germs, you might touch a doorknob. And then you sit there. You don't wash your hands. Your anxiety spikes. It hits the ceiling. You feel like you're going to die or puke. But then, slowly, the anxiety drops. Your brain learns that the "danger" wasn't real. This is called habituation.
Medications, specifically SSRIs (Selective Serotonin Reuptake Inhibitors) like Zoloft or Prozac, can also help by "lowering the volume" of the intrusive thoughts so the therapy can actually work.
Nuance: It’s a Spectrum
OCD isn't binary. You don't either "have it" or "not have it" in a way that looks the same for everyone. Some people have mild symptoms that take up an hour a day. Others are completely housebound.
There are also related disorders that fall under the "OCD Umbrella," like:
- Body Dysmorphic Disorder: Obsessing over perceived flaws in physical appearance.
- Hoarding Disorder: Difficulty discarding possessions regardless of value.
- Trichotillomania: The urge to pull out one's hair.
- Excoriation: Skin picking.
How to Actually Help Someone
If someone tells you they have OCD, don't ask them to come over and clean your house. Seriously. It’s not funny.
The best thing you can do is listen without judgment. Don't provide constant reassurance. If they ask, "Do you think I'm a bad person?" for the fiftieth time, saying "No, of course not" actually feeds the OCD cycle. It gives a temporary hit of relief that reinforces the need to ask again later. Instead, experts suggest saying something like, "That's your OCD talking, and I'm not going to answer that because I want to help you get better." It feels mean, but it's the kindest thing you can do.
Actionable Steps for Moving Forward
If you suspect you or someone you love is struggling with what OCD actually is, here is how you start the journey back to reality:
- Get a proper screening. Don't self-diagnose via TikTok. Use a tool like the Yale-Brown Obsessive Compulsive Scale (Y-BOCS), which is the industry standard for measuring symptom severity.
- Find a specialist. General talk therapy (just venting about your childhood) often doesn't work for OCD and can sometimes make it worse. You need someone specifically trained in ERP (Exposure and Response Prevention).
- Check the International OCD Foundation (IOCDF). Their website is basically the Bible for this condition. They have a directory of therapists who actually know what they’re doing.
- Be patient. Recovery isn't linear. There will be days where the "brain noise" is deafening. That doesn't mean the treatment isn't working; it just means it's Tuesday.
Understanding what does OCD mean is the first step toward stripping away the stigma. It is a medical condition, a neurological hiccup, and a heavy burden—but with the right tools, the "broken record" in the brain can finally be silenced.
Resources for Immediate Help
- International OCD Foundation (IOCDF): iocdf.org
- Crisis Text Line: Text HOME to 741741
- NAMI (National Alliance on Mental Illness): 1-800-950-NAMI (6264)