You’re standing in front of the mirror, or maybe you're just sitting on the edge of the tub after a long day, and you see them. Those twisty, bulging, slightly bluish ropes snaking down your calf or behind your knee. Most people just think they’re an eyesore—a tax you pay for getting older or standing too long at work. But then you start wondering. Is that dull ache normal? Why does that one spot feel warm? Honestly, knowing when to worry about varicose veins is the difference between a simple lifestyle tweak and a midnight run to the ER.
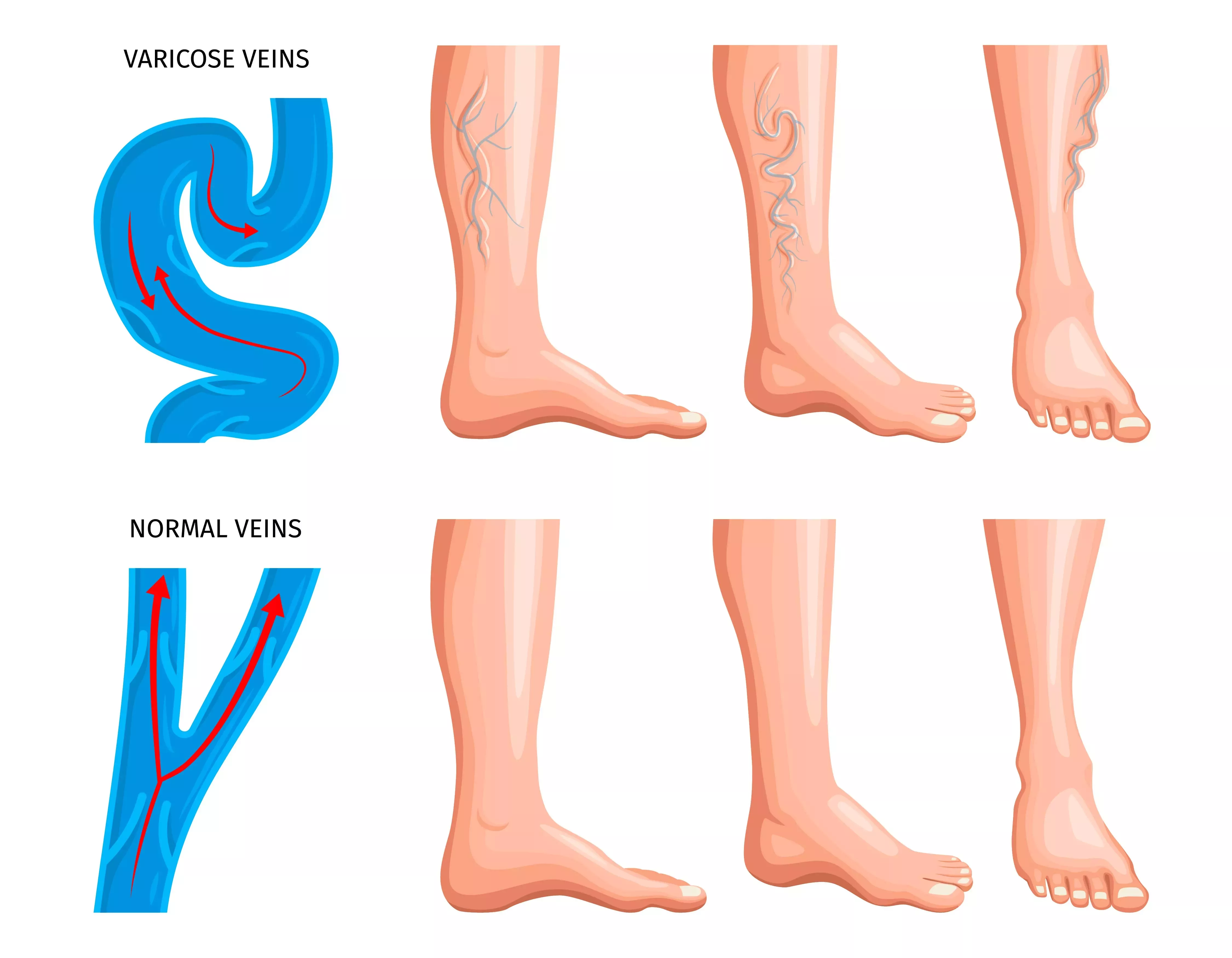
Most of the time, these veins are just a nuisance. They’re basically just veins that have lost their "oomph." The tiny valves that are supposed to push blood back up toward your heart start failing, and gravity wins. Blood pools. The vein stretches. It looks gnarly. But "gnarly" isn't always "dangerous."
Here is the thing: your vascular system is a closed loop. If one part of the plumbing is backed up, it creates pressure elsewhere. While you might be tempted to just wear longer pants and forget about it, your body usually drops hints when things are shifting from a cosmetic "oops" to a medical "uh-oh."
💡 You might also like: How Much Oxygen Do We Breathe? The Surprising Reality of Every Breath
The red flags that mean it's time for a doctor
If your legs feel heavy, like you’re wading through wet concrete by 4:00 PM, that’s a classic symptom. It’s annoying, sure. But it’s not necessarily an emergency. However, if you notice spontaneous bleeding from a vein, that is a massive red flag. The skin over a varicose vein gets thin over time. Sometimes, even a minor bump or just the pressure itself can cause the vein to pop. It can bleed a lot. If that happens, elevate your leg, apply pressure, and get to a clinic.
You should also be looking for skin changes. This is something people miss constantly. If the skin around your ankle starts looking dark, leathery, or reddish-brown, that’s not a tan. It’s called stasis dermatitis. It happens because blood is literally leaking out of your capillaries and staining your tissue. If you ignore this, the skin can eventually break down into a venous ulcer. Those are incredibly hard to heal and painful as hell.
Then there’s the heat. If one specific area of a bulging vein feels hot to the touch, red, and tender, you might be looking at superficial thrombophlebitis. Basically, a small clot has formed in that surface vein. While these aren't usually the "deadly" kind of clots, they can migrate to the deeper system if you don't treat them.
Deep Vein Thrombosis (DVT): The real danger
We can't talk about when to worry about varicose veins without mentioning DVT. This is the big one. This is the "call 911" territory. While varicose veins are in the superficial system, they can be a sign that your overall venous health is struggling. If you experience sudden, massive swelling in just one leg—not both—accompanied by a cramping pain that feels like a charley horse that won't go away, you need an ultrasound immediately.
If that clot breaks loose, it travels to the lungs. That's a pulmonary embolism.
Signs of that?
- Sudden shortness of breath.
- Chest pain when you breathe deeply.
- Coughing up blood.
- A sense of impending doom.
Seriously, if your leg is swollen like a balloon and you’re struggling to catch your breath, stop reading this and go to the hospital.
Why some people get them and others don't
It's partly luck. Well, genetic luck. If your mom and grandma had legs that looked like a roadmap of the tristate area, you’re probably going to have them too. According to the Society for Vascular Surgery, about 20% to 30% of adults will deal with this at some point.
Pregnancy is another huge factor. You’ve got way more blood pumping through your body, and the hormone progesterone relaxes vein walls. Plus, a whole human is sitting on the veins in your pelvis. It's a perfect storm for venous insufficiency. Usually, pregnancy-related veins get better a few months after delivery, but not always.
Occupations matter. Teachers, nurses, retail workers—basically anyone who stands on hard floors for eight hours a day—are at the highest risk. Your calf muscles act as a secondary pump for your heart. When you stand still, that pump is off. The blood just sits there, stretching the vein walls until the valves can't meet in the middle anymore.
Myths about varicose veins we need to bury
Can you get them from crossing your legs?
Nope.
That's an old wives' tale. Crossing your legs might make an existing problem feel slightly more uncomfortable because you're adding pressure, but it isn't the root cause.
What about running? Some people think the impact causes veins to "pop." In reality, running is great for your veins because it engages the calf pump. The only caveat is if you already have severe reflux, you might want to wear compression socks while you log those miles to keep the blood moving in the right direction.
Another big misconception is that "only old people get them." I've seen athletes in their 20s with bulging varicosities. If you have a genetic predisposition or a history of leg trauma, age is just a number. The "worry" factor is the same whether you're 25 or 75.
Non-surgical ways to manage the ache
Before you go under the laser, there are things you can do at home. Honestly, most insurance companies won't even pay for a procedure until you’ve tried "conservative management" for three to six months anyway.
- Compression is king. Get medical-grade stockings (20-30 mmHg). Not the cheap ones from the drugstore. You want the ones that are tighter at the ankle and get looser as they go up. They squeeze the veins and help the valves close.
- Elevate. And I don't mean just putting your feet on an ottoman. Your ankles need to be above your heart. Gravity is your enemy all day; make it your friend for 20 minutes every evening.
- Move. If you sit at a desk, do toe heels. Flex your feet. If you stand, pace around. Just keep those calves firing.
- Watch the salt. Sodium makes you retain water, which adds volume to your blood and pressure to your veins.
When the "home stuff" isn't enough
If you’ve tried the socks and the elevation and your legs still feel like they're on fire at the end of the day, it's time to see a vascular specialist. They’ll usually do a duplex ultrasound. It’s painless. They just use a wand to look at the blood flow and see exactly which valves are leaking.
Modern treatments aren't like the "vein stripping" your grandma had. That was brutal. Nowadays, it’s mostly endovenous laser ablation (EVLT) or radiofrequency ablation. They basically use heat to seal the bad vein shut. Your body naturally reroutes the blood to healthier veins deeper in the leg. You’re usually up and walking the same day. There’s also sclerotherapy, where they inject a foam or liquid into smaller veins to make them collapse and fade away.
Actionable steps for your leg health
If you are currently looking at your legs and wondering when to worry about varicose veins, follow this checklist to decide your next move.
First, do a visual and tactile check. Are there sores near your ankles that won't heal? Is the skin hard or discolored? If yes, book an appointment with a vascular surgeon this week.
Second, monitor the pain. Is it a dull ache that goes away when you walk or elevate, or is it a sharp, localized pain that hurts even when you're resting? Persistent, localized pain needs a professional look.
Third, check for asymmetry. Both legs swelling is often a heart or kidney issue or just a salty dinner. One leg swelling is a vascular "check engine" light.
Finally, if you’re just bothered by how they look, that’s valid too. You don't have to wait for a medical emergency to seek treatment. Heavy, tired legs might be "normal" for you, but they don't have to be. Improving your venous circulation can significantly boost your energy levels and overall quality of life.
- Audit your footwear: Switch from high heels to flats to allow your calf muscles to work properly.
- Measure for socks: Use a tape measure to get your ankle and calf circumference before buying compression gear to ensure it actually works.
- Schedule a screening: If you have a family history, getting a baseline ultrasound in your 30s or 40s can help you catch issues before they turn into ulcers or clots.
- Hydrate: Keeping your blood viscosity low helps it move more easily through narrowed or damaged vessels.
Take care of your legs now. You’ve only got one pair, and they’ve got a lot of miles left to cover.