You’re sitting in the doctor’s office. The cuff squeezes your arm until it pulses. The nurse reads off two numbers, and suddenly you’re staring at a screen wondering why is my bottom blood pressure number high when the top one looks totally fine. It’s confusing. Most of the health advice we hear focuses on the top number—the systolic—as the "big one" to watch out for as we get older. But that bottom number, the diastolic pressure, has its own story to tell. If your reading looks something like 115/95, you’ve stepped into the world of isolated diastolic hypertension (IDH).
It’s actually kinda common in younger adults. While the medical community spent decades obsessed with systolic pressure, recent data suggests the diastolic reading is a major red flag for certain types of cardiovascular stress.
Understanding the "Resting" Pressure
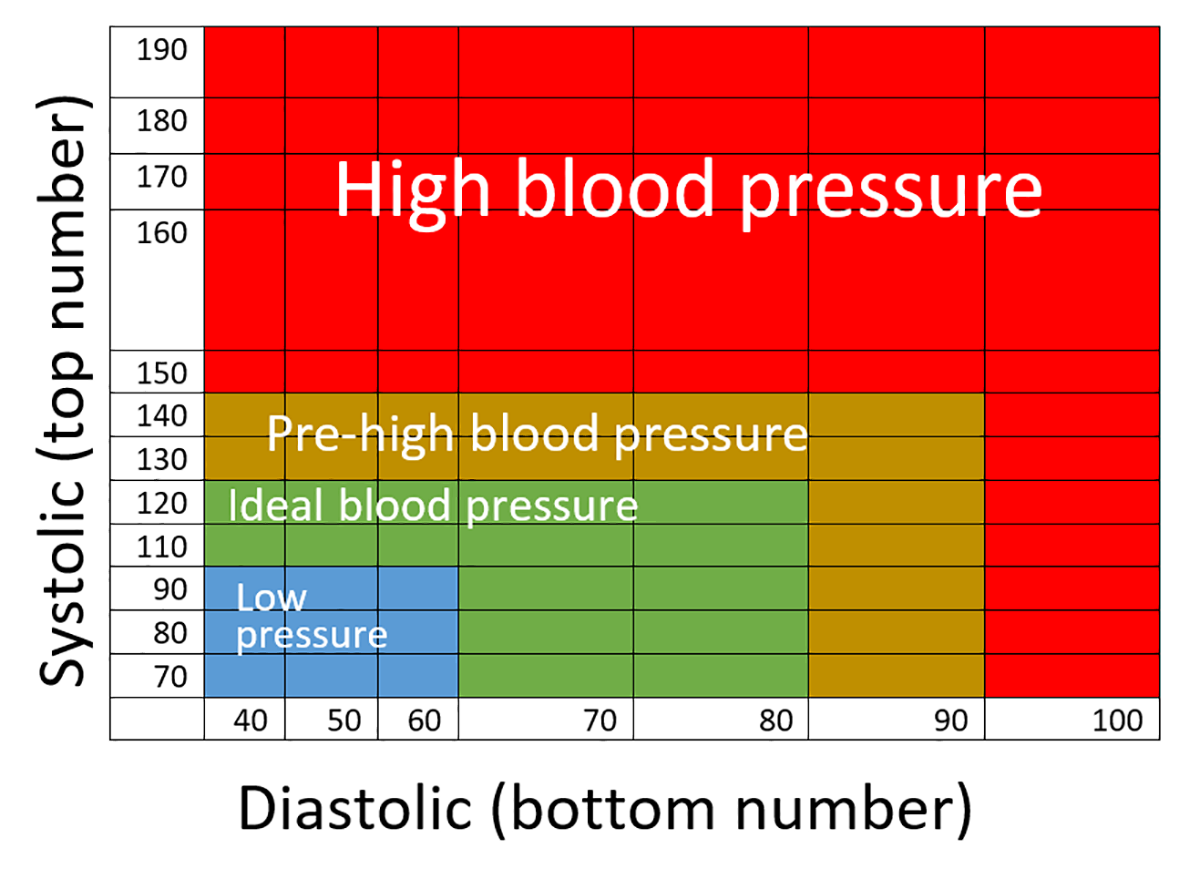
Let’s get the basics straight. Blood pressure is essentially a measure of how much force your blood is putting on your artery walls. The top number (systolic) is the pressure when your heart beats. The bottom number (diastolic) is the pressure in your arteries when your heart is resting between beats.
Think of it like a garden hose. If you turn the nozzle off but the water is still pushing hard against the rubber, that’s diastolic pressure. If that pressure stays high, your arteries never get a "break." They are under constant tension. According to the American College of Cardiology and the American Heart Association, a diastolic reading of 80 mmHg or higher is considered elevated. If it hits 90 or above, you’re officially in Stage 2 hypertension territory, even if your top number is a perfect 110.
Why does this happen? Usually, it's because the smaller blood vessels in your body, the arterioles, have become stiff or narrow. They are resisting the flow of blood. This resistance keeps the pressure high even when the heart isn't actively pumping. It's often a sign that your body's "plumbing" is tighter than it should be.
The Usual Suspects: Lifestyle and Biology
If you’re wondering why is my bottom blood pressure number high, the answer often lies in metabolic health. Younger men and women are the primary demographic for isolated diastolic hypertension.
✨ Don't miss: Human Body All Organs Explained: Why Your Spleen and Skin Matter More Than You Think
Weight is a massive factor. It's not just about the scale, but specifically where you carry the weight. Excess abdominal fat releases inflammatory chemicals that can cause blood vessels to constrict. This isn't just theory; it’s a physiological reality. Then there's the salt. Modern diets are packed with sodium, which causes the body to retain fluid. More fluid in the pipes means more pressure.
Alcohol is another big one. You might think a few drinks help you relax, but alcohol actually stimulates the sympathetic nervous system. This is the "fight or flight" response. When it's overstimulated, your blood vessels tighten up, and that diastolic number creeps upward.
Stress matters too. Honestly, we underestimate it. Chronic stress keeps your cortisol levels high. High cortisol leads to narrowed arteries. If you're constantly "on" at work or home, your bottom number might be reflecting that internal tension. It’s your body’s way of saying it can’t find a moment of peace, even between heartbeats.
Is it your medication?
Sometimes the culprit is in your medicine cabinet. Some over-the-counter drugs can spike diastolic pressure.
- NSAIDs: Ibuprofen and naproxen can cause your body to hold onto salt and water.
- Decongestants: Anything with pseudoephedrine works by narrowing blood vessels—including the ones in your arm.
- Certain Antidepressants: Specifically SNRIs can occasionally nudge that bottom number up.
The Risks: It’s Not Just a Number
For a long time, doctors thought isolated diastolic hypertension was "benign." They figured as long as the systolic was low, you were safe. We now know that's not true. A study published in JAMA involving over 1.3 million people showed that while systolic pressure has a bigger impact on overall heart disease, diastolic pressure is a strong predictor of abdominal aortic aneurysms.
✨ Don't miss: Preparing for anal sex: What most people get wrong about getting ready
If that bottom number stays high for years, it can damage the small vessels in your kidneys and eyes. It’s a silent, steady pressure. It's like a tire that's overinflated; eventually, something gives.
How to Actually Lower That Bottom Number
Fixing high diastolic pressure isn't just about "eating better." It requires a specific approach to relaxing the vascular system.
Magnesium is your best friend. It’s a natural calcium channel blocker. It helps the smooth muscles in your blood vessel walls actually relax. Most people are deficient in it. Foods like spinach, pumpkin seeds, and almonds are great, but some people find a high-quality magnesium glycinate supplement makes a noticeable difference in their diastolic readings within weeks.
Stop the constant snacking. This might sound weird for blood pressure, but it’s about insulin. High insulin levels tell your kidneys to hold onto sodium. By practicing time-restricted eating (like an 8-hour window), you lower your baseline insulin, which allows your body to flush out excess salt and fluid. It’s an indirect but powerful way to drop that bottom number.
Get moving, but don't just do cardio. While running is great for your heart, resistance training has a unique effect on vascular health. When you lift weights, your muscles produce nitric oxide. Nitric oxide is a vasodilator—it literally tells your arteries to "open up."
The White Coat Effect
Before you panic, make sure your reading is real. Many people experience "white coat hypertension." Your heart rate goes up and your vessels tighten just because you're in a medical setting.
👉 See also: Black Women Having Sex: Reclaiming Pleasure and Navigating the Healthcare Gap
To get an accurate answer to why is my bottom blood pressure number high, you need to track it at home. Buy a validated upper-arm cuff. Sit quietly for five minutes before taking a reading. Don't talk. Don't look at your phone. Keep your feet flat on the floor. Take three readings and average them. If the number is still high in your living room, then it’s time to take action.
Practical Next Steps
If you’ve confirmed that your diastolic pressure is consistently hitting 85 or 90+, don't just wait for your next annual checkup.
- Audit your salt intake for 48 hours. You'll be shocked at how much sodium is in "healthy" foods like bread and salad dressing. Aim for under 1,500mg a day for a week and see if the number budges.
- Check your sleep. Obstructive Sleep Apnea is a massive driver of high diastolic pressure. If you snore or wake up tired, your oxygen levels might be dropping at night, causing your blood pressure to spike while you sleep.
- Increase potassium. Potassium works as the "antidote" to sodium. It helps the body excrete salt and eases tension in the blood vessel walls. Avocado, bananas, and potatoes (with the skin!) are the easiest ways to get it.
- Talk to a professional about a "metabolic panel." Ask for your fasting insulin and C-reactive protein levels. This will tell you if inflammation or insulin resistance is the root cause of your stiff arteries.
Isolated diastolic hypertension is a signal. It's a warning from your peripheral vascular system that it’s under too much strain. The good news? Because it's often caught in younger people, it's incredibly responsive to lifestyle shifts. You can often bring that number back into the 70s just by changing how you move and what you put on your plate.