Most people think of "Mono" as a high school rite of passage. You get a fever, your throat feels like it’s full of glass, you sleep for three weeks, and then it's over. But that's not how it works. Once you’ve had the Epstein-Barr virus (EBV), it stays. It’s a literal squatter in your B-cells for the rest of your life. For most of us, the immune system keeps it in "jail" indefinitely. However, things can change. When the immune system wavers, you get reactivation of Epstein Barr virus, and honestly, it doesn't look anything like the first time you caught it.
It's subtle. It’s a weird, persistent fatigue that caffeine won't touch. It’s brain fog that makes you forget why you walked into a room. Because it doesn't always come with a raging fever or swollen glands, doctors often miss it entirely.
🔗 Read more: What Helps With Teething: Real Relief That Isn't Just Freezing a Washcloth
The Science of a Sleeping Giant
EBV is a member of the herpesvirus family. Just like its cousins—cold sores and shingles—it specializes in latency. It basically hides its DNA inside your own cells, waiting for a moment of weakness. When we talk about reactivation of Epstein Barr virus, we aren't talking about "catching" it again. You already have it. About 95% of adults do.
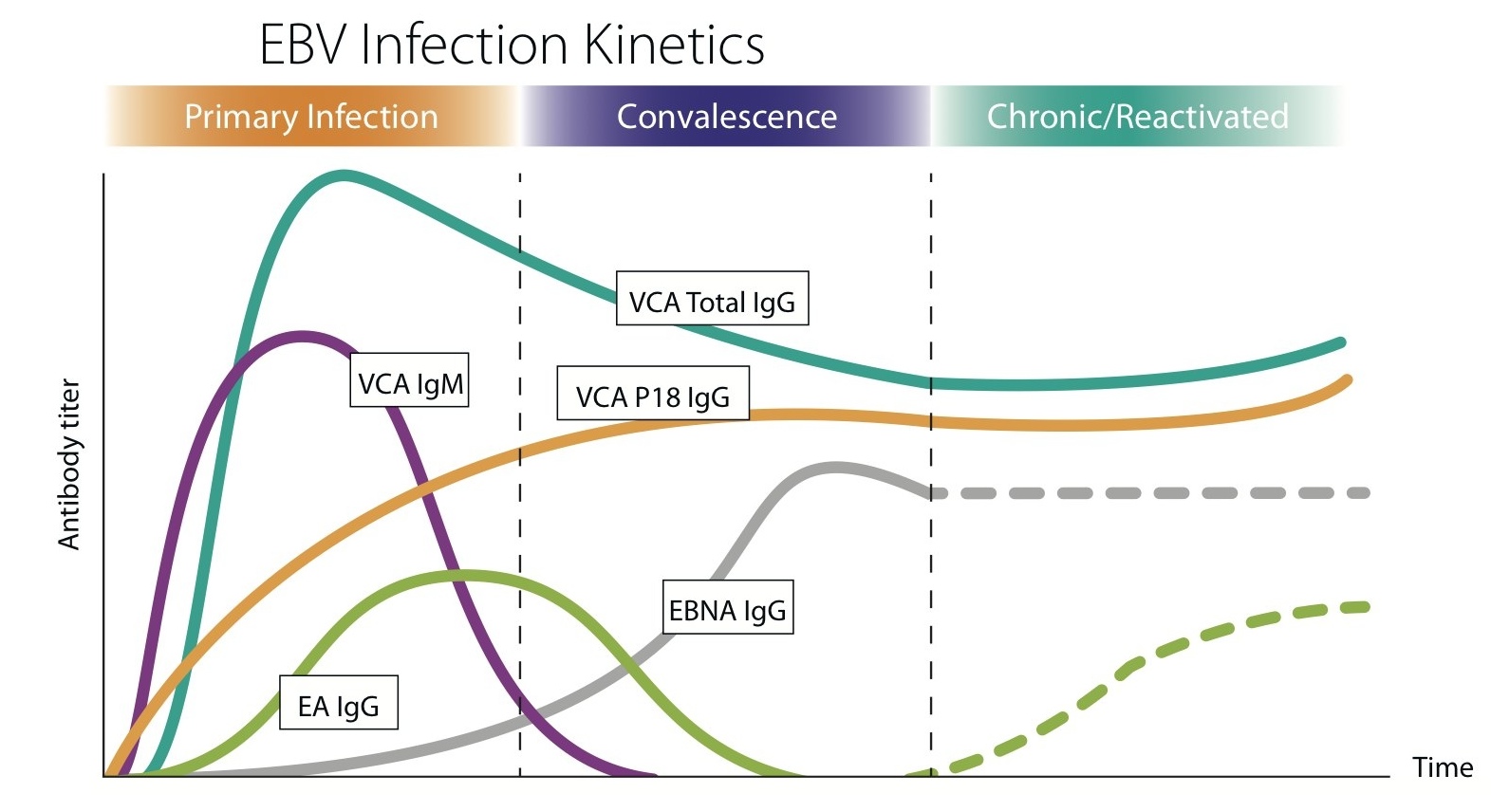
The reactivation happens when the lytic cycle is triggered. This is the phase where the virus stops sleeping and starts replicating. It begins pumping out viral proteins like EBNA-1 (Epstein-Barr nuclear antigen 1) and EA-D (Early Antigen). These aren't just technical terms; they are the literal markers doctors look for in blood work to see if the virus is currently active.
Why does this happen? Stress is the big one. And I don't just mean "I had a bad day at work" stress. I mean the physiological toll of major life trauma, lack of sleep, or another infection. Recently, researchers have been looking at how other viruses, like the one that causes COVID-19, act as a "tripwire" for EBV. A study published in the journal Pathogens found that a significant portion of Long COVID patients actually showed signs of reactivation of Epstein Barr virus. It’s like the new infection distracted the "guards" (your T-cells), and EBV just walked right out of the cell's nucleus and started making trouble.
What Reactivation Actually Feels Like
If you go to a doctor and say "I'm tired," they'll check your thyroid. They'll check your iron. They might tell you to drink less wine or get an extra hour of sleep. If those things are fine and you still feel like you’re walking through waist-deep mud, EBV might be the culprit.
Reactivation doesn't always mirror the acute Mononucleosis phase. You might get:
- A "hangover" feeling without drinking.
- Lymph nodes that feel tender but aren't visibly swollen.
- A low-grade "buzzing" or malaise that fluctuates throughout the day.
- New or worsening sensitivities to certain foods.
- Muscle aches that feel like you ran a marathon when you actually just sat at a desk.
It’s frustrating. Truly. Because these symptoms are "non-specific," they get lumped into "burnout" or "aging." But there is a biological mechanism at play here. When the virus reactivates, it triggers a cytokine storm—on a micro-scale. Your body is stuck in an inflammatory loop.
The Autoimmune Connection
This is where it gets a bit heavy. We used to think EBV was just an annoyance. Now, we know it's a major player in autoimmune diseases. Dr. Alberto Ascherio and his team at Harvard published a massive study in Science (2022) involving 10 million military personnel. The findings were staggering: EBV is likely the primary cause of Multiple Sclerosis (MS).
It’s called molecular mimicry. Basically, the virus looks so much like certain proteins in your body that your immune system gets confused. It tries to attack the virus but ends up attacking your myelin sheath or your thyroid gland instead. This is why managing reactivation of Epstein Barr virus isn't just about feeling less tired—it’s about long-term systemic health.
💡 You might also like: Potato in Calories: Why You’ve Been Lied to About Spuds
Testing: Don't Let Them Give You the Wrong Panel
If you suspect your EBV is acting up, you have to be specific with your doctor. Most labs only run an "EBV Screen" which just tells you if you've ever had it. Since almost everyone has, that test is useless for diagnosing a current flare-up.
You need the EBV Acute Panel. Specifically, look for these four markers:
- VCA IgM: This usually indicates a brand-new infection. Rare in adults, but possible.
- VCA IgG: This just means you’ve had it in the past. By itself, it doesn't mean much.
- Early Antigen (EA-D) IgG: This is the "smoking gun." If this is high, the virus is likely replicating right now.
- EBNA IgG: This shows up months after an infection.
If your VCA IgG and EBNA are high, but EA-D is low, you’re likely in the "latent" phase. You’re fine. But if that EA-D is elevated alongside symptoms, you’re dealing with an active reactivation.
Why Me? The Triggers Nobody Mentions
It isn't just "stress." That's a cop-out answer. We need to look at the specific physiological "keys" that unlock the virus.
Nutritional deficiencies are a massive, overlooked factor. The immune system needs specific raw materials to keep a virus suppressed. Vitamin D is the most critical. Low Vitamin D levels are consistently linked to higher EBV viral loads. If you're "borderline" on your lab results, that might not be enough for your T-cells to do their job. Selenium and Zinc are also vital. Without them, your "natural killer" cells—the ones that literally hunt down virus-infected cells—become sluggish.
Then there is the gut-brain-virus axis. We know that gut dysbiosis (an imbalance of bacteria) causes systemic inflammation. This inflammation signals to the dormant EBV that the body is under stress, which can trigger the lytic cycle. It's all connected. You can't treat the virus without looking at the host.
Real Talk on Recovery and Management
There is no "cure" for EBV. No magic pill. Acyclovir and other antivirals are sometimes prescribed, but the evidence for them working on EBV is actually pretty weak compared to how they work on shingles.
So, what do you actually do? You make your body a "hostile environment" for the virus.
First, you have to stop the "push-crash" cycle. If you have reactivation of Epstein Barr virus, you cannot exercise your way out of it. Intense cardio is like pouring gasoline on the fire. It spikes cortisol, which further suppresses the immune response that’s trying to kill the virus. Switch to walking or restorative yoga until your EA-D levels drop.
Diet matters, but not in a "fad" way. You need high lysine and low arginine. Arginine is an amino acid that the herpes family of viruses uses to replicate. Chocolate, nuts, and seeds are high in arginine. I'm not saying never eat an almond again, but if you're in a flare, maybe back off the trail mix. Focus on lean proteins and a mountain of colorful vegetables to provide the polyphenols your immune system is screaming for.
Specific Interventions That Work
- Monolaurin: This is a fatty acid derived from coconut oil. It has been shown in some in vitro studies to disrupt the lipid envelope of viruses. Many people with chronic EBV find it life-changing, though you should start with a tiny dose to avoid a "die-off" reaction (Herxheimer response).
- Adaptogens: Herbs like Ashwagandha or Rhodiola help modulate the stress response. If you can keep your cortisol stable, your immune system stays in the driver's seat.
- Sleep Hygiene: This isn't optional. EBV replication is often suppressed during deep sleep cycles when T-cell activity peaks. If you're getting six hours of crappy sleep, you're basically giving the virus a green light.
The Mental Toll of a "Ghost" Illness
One of the hardest parts of reactivation of Epstein Barr virus is that you look fine. Your coworkers won't understand why you're exhausted. Your partner might think you're just being "lazy." This leads to a secondary layer of depression and anxiety, which—you guessed it—further weakens the immune system.
Acknowledge that this is a real, biological event. It isn't in your head. The medical community is finally catching up, thanks to the massive influx of research into post-viral syndromes. You aren't crazy; you're just hosting a very demanding biological guest.
💡 You might also like: People with two heads: The real science and lives behind the headlines
Moving Forward: Your Action Plan
If you think you're dealing with this, don't just guess. Knowledge is the only way to stop the spiral.
Start by getting the full EBV panel mentioned above. Don't let the lab skip the Early Antigen (EA) test. Once you have those numbers, look at your Vitamin D levels. If they are below 50 ng/mL, talk to a professional about aggressive supplementation.
Audit your stress. Not the "I can handle it" kind of stress, but the physical reality of your schedule. If you are in a reactivation phase, you have to prioritize rest over productivity. It’s a hard pill to swallow in a culture that prizes "the grind," but the virus doesn't care about your deadlines.
Finally, consider working with a functional medicine practitioner who understands viral load management. They can help you look at co-infections like Mold or Lyme, which often hang out with EBV like a bad crowd. Clean up your environment, support your mitochondria, and give your immune system the tools it needs to put the virus back to sleep. You can get your energy back, but you have to stop fighting the symptoms and start addressing the viral reactivation at its root.