You’re tired. Really tired. Between the middle-of-the-night feedings and the general haze of new parenthood, the eight-week mark sneaks up on you fast. Then comes the pediatrician’s reminder about the 2 month vaccination schedule, and suddenly, there’s this weird mix of relief that you’re protecting them and total dread about the needles. It’s a lot. Most parents I talk to feel a bit overwhelmed by the sheer number of shots happening at once. Honestly, it looks like a lot for such a tiny human, but there is a very specific, science-backed reason why the CDC and the American Academy of Pediatrics (AAP) stack them this way.
The immune system of an eight-week-old is like a blank canvas, but it’s also vulnerable. They’ve lost some of that initial "passive immunity" they got from mom in the womb, and now they need to start building their own defenses. We aren't just guessing here. Decades of data from the CDC’s Pink Book show that this specific timing catches babies right before they are most likely to be exposed to some pretty nasty bugs.
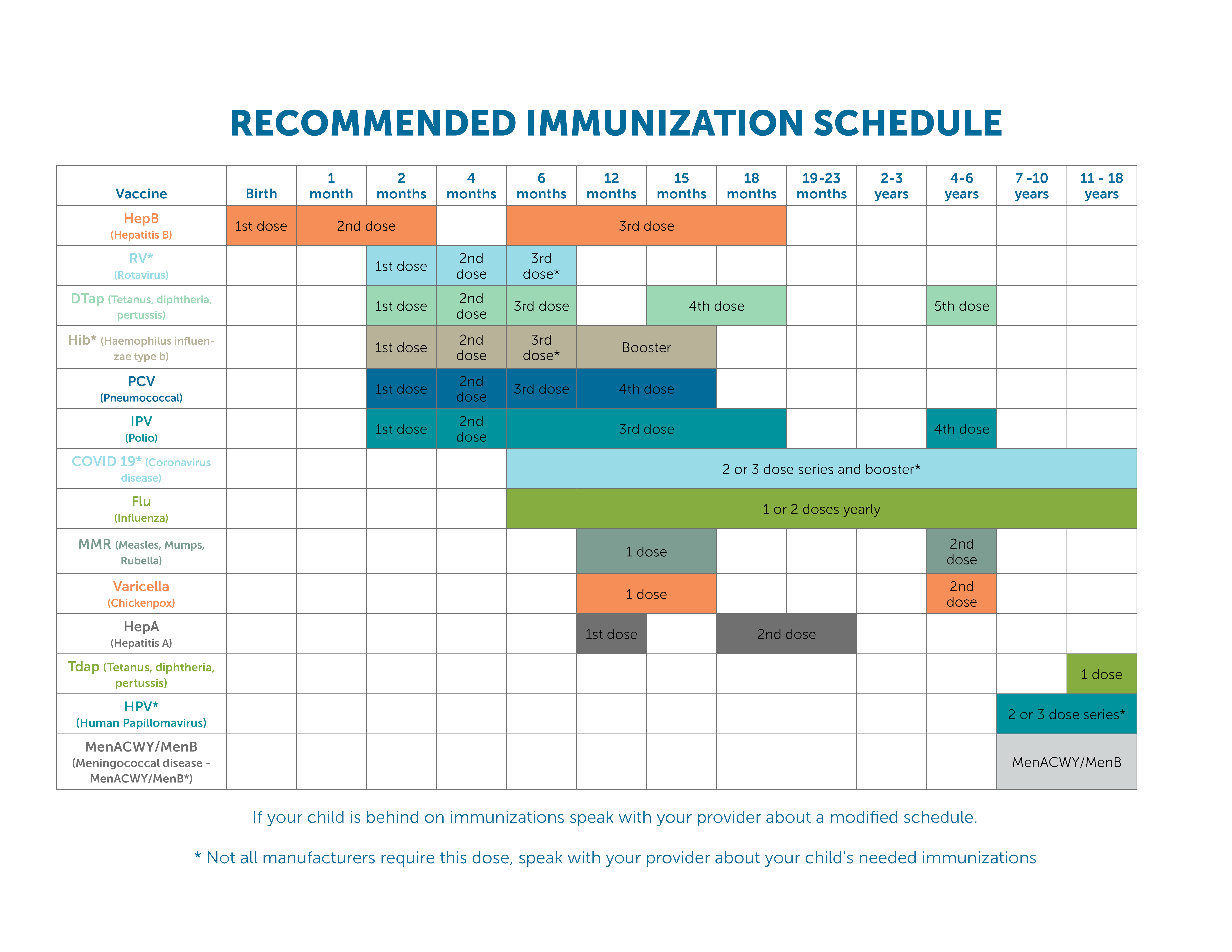
What is actually in the 2 month vaccination schedule?
It isn't just one shot. It’s usually a series of injections and one oral drop. If your doctor uses combination vaccines like Pediarix, it might only be two or three pokes, which is a lifesaver for your nerves.
First up is Rotavirus (RV). This one is unique because it’s a liquid they swallow. Rotavirus is basically the king of "stomach flu" in babies, causing severe diarrhea and dehydration. Then you have DTaP, which covers Diphtheria, Tetanus, and acellular Pertussis (whooping cough). Whooping cough is the big one here. For an adult, it’s a nagging cough; for a two-month-old, it can be life-threatening because their airways are so small.
👉 See also: Why Are Men Smarter Than Women: What the Science Actually Says About Brain Differences
Next is the Haemophilus influenzae type b (Hib) vaccine. Don't let the name fool you—it’s not the flu. Hib used to be the leading cause of bacterial meningitis in kids under five. Since the vaccine rollout, those cases have plummeted by over 99%. Then there’s the Pneumococcal conjugate vaccine (PCV13 or PCV15), which fights off bacteria that cause ear infections, pneumonia, and blood infections. Finally, there's Inactivated Poliovirus (IPV) and a second dose of Hepatitis B, if they didn't already get the second dose at the one-month mark.
Why so many at once?
I get it. You look at that tiny thigh and think, is this too much for their immune system? Basically, no.
Scientists like Dr. Paul Offit from the Children’s Hospital of Philadelphia have pointed out that a baby’s immune system handles thousands of "antigens" (the stuff that triggers an immune response) every single day just by breathing and eating. The total number of antigens in the entire 2 month vaccination schedule is a literal drop in the bucket compared to what they face crawling on a rug or sticking a fist in their mouth.
Splitting them up—what some call an "alternative schedule"—actually increases the risk. It leaves the baby unprotected for longer and, quite frankly, means more trips to the doctor and more stressful "shot days" for both of you. It’s better to get the protection started early.
The side effects nobody tells you about (and what’s normal)
Most parents expect a fever. And yeah, about 25% of babies get a mild one. Their legs might be a bit red or swollen where the needle went in. That’s just the body building its "memory" of the germs.
But there’s also the "post-vax funk." Your baby might be incredibly sleepy for 24 hours. Or, they might be the opposite—fussy, clingy, and impossible to put down. Honestly, it’s a bit of a coin flip. I’ve seen babies sleep through the whole night after their two-month shots, and I’ve seen babies scream if you even look at their legs.
Pro tip: Don’t give Tylenol (acetaminophen) before the shots unless your doctor specifically tells you to. Some studies suggest it might slightly dampen the initial immune response. Wait until after the shots to see if they actually need it for a fever or significant discomfort. Always check the dosage with your pediatrician first, because it’s based on weight, not age.
Addressing the "aluminum" and "preservatives" talk
If you’ve spent any time on social media, you’ve seen the posts about "heavy metals." It’s scary-sounding stuff. But let’s look at the actual chemistry.
Aluminum salts are used as "adjuvants." This is just a fancy way of saying they help the vaccine work better so we can use a smaller amount of the actual virus or bacteria. You actually find more aluminum in standard breast milk or infant formula than what is in a vaccine. Babies are born with aluminum already in their systems, and they clear it out through their kidneys quite efficiently.
As for thimerosal (the mercury-based preservative)? It hasn't been in routine childhood vaccines (except some multi-dose flu vials) since 2001. So, that’s a non-issue for the 2 month vaccination schedule.
Survival tactics for the appointment
The actual "poke" lasts about five seconds. The buildup is way worse for you than it is for them.
- Sweet-Ease: Some clinics have sucrose (sugar water) drops. It’s like magic for distracting babies from pain.
- The "Shush-Pat": Be ready to feed or cuddle immediately. Skin-to-skin contact releases oxytocin, which is a natural pain reliever.
- Leggings vs. Snaps: Wear an outfit that is easy to remove. Snaps are your friend; tight skinny jeans on a baby are a nightmare when the nurse is waiting.
- The Nursing Tuck: If you are breastfeeding, many doctors allow you to nurse during the shots. It’s often the fastest way to calm them down.
What to watch for after you get home
Most reactions are "local" (at the site) and "systemic" (fever/fussiness). But you should know the red flags. If your baby has a fever over 100.4°F (38°C) that doesn't budge with Tylenol, or if they are "inconsolable"—we’re talking high-pitched screaming for more than three hours—call the office.
Anaphylaxis (a severe allergic reaction) is incredibly rare, occurring in about one per million doses. It usually happens within minutes of the shot, which is why most clinics have you wait in the lobby for 15 minutes before leaving. If you’re home and you see hives or difficulty breathing, that’s an ER visit. But again, the odds are astronomical.
Actionable steps for your 8-week visit
Don't go in blind. Being prepared makes the day go ten times smoother.
- Check your records. Make sure you know if your baby got their second Hep B shot yet. Some hospitals give it at birth, some at one month.
- Verify the combo. Ask your doctor if they use combination vaccines like Vaxelis or Pediarix to reduce the total number of injections.
- Prep the medicine cabinet. Have infant-strength acetaminophen on hand, but don't use it until after the appointment if symptoms arise.
- Mark the calendar. The next round is at four months. Most clinics will book this before you leave the parking lot.
- Watch the legs. Apply a cool, damp cloth to the injection sites if they look red or feel firm later that evening.
The 2 month vaccination schedule is a major milestone. It’s the first big step in moving away from that "newborn bubble" and into a world where they have their own internal shield against some of the most dangerous diseases in history. It’s a tough afternoon, but the peace of mind is worth the couple of hours of extra cuddles.